eISSN: 2373-6372


Research Article Volume 13 Issue 1
1Department of General Surgery, Nuevo Hospital Civil de Guadalajara “Juan I. Menchaca”, México
2Centro Universitario de Ciencias de la Salud, Universidad de Guadalajara, México
3Department of General Surgery, Antiguo Hospital Civil de Guadalajara “Fray Antonio Alcalde”, México
4Department of General Surgery, Hospital General de Occidente, México
Correspondence: Itzé Aguirre-Olmedo. Department of General Surgery. Universidad de Guadalajara Nuevo Hospital Civil de Guadalajara “Juan I. Menchaca”. Salvador Quevedo y Zubieta 750, Independencia Oriente, C.P. 44340, Guadalajara, Jalisco, México, Tel +52 333942 4400
Received: October 07, 2021 | Published: January 11, 2022
Citation: Aguirre-Olmedo I, Rea-Alvarez SDC, Nuño-Guzmán CM, et al. Gallstone ileus diagnosis and treatment: six-year experience in three academic institutions. Gastroenterol Hepatol Open Access. 2022;13(1):1-8. DOI: 10.15406/ghoa.2022.13.00486
Background: Gallstone ileus is defined as a mechanical intestinal obstruction due to impaction of one or more gallstones within the gastrointestinal tract. It occurs most frequently in elderly patients, and accounts for 1%-4% of mechanical intestinal obstructions. The mainstay of treatment is surgical exploration.
Methods: We present a retrospective review of patients with gallstone ileus, treated during 2015-2020, in three western academic centers in Mexico. The aim of this study was to describe the clinical manifestations, radiological and operative findings, surgical treatment and postoperative outcomes.
Results: The study included sixteen patients. Seventy five percent of patients were female and the overall median age was 55 years (range 26-81). Clinical presentation included abdominal pain (93.7%), vomit (81.2%), abdominal distention and impossibility to pass feces and flatus (68.7%). Classical image findings were observed on plain abdominal radiographs (43.7%), ultrasound (37.5%) and computed tomography (81.2%). All patients underwent surgical treatment. The terminal ileum was the most common site of impaction (75%). The most frequent fistula was cholecystoduododenal (75%). Enterotolithotomy alone was performed in 68.7% of patients, and one-stage-procedure in 31.2%. Overall morbidity rate and morality rates were 75% and 12.5%, respectively.
Conclusions: Gallstone ileus is a rare cause of gastrointestinal obstruction, with female and elderly population preponderance, although younger patients are affected. A high clinical index of suspicion guides image modality selection, where CT is the most useful image used. Enterolithotomy alone is the most frequent surgical approach, with a lower morbidity rate. Indications for a one-stage surgical approach remain to be established.
Keywords: biliary fistula, ileus, biliary calculi, intestinal obstruction, cholelithiasis
Gallstone ileus (GI) is an infrequent complication of cholelithiasis and is defined as a mechanical intestinal obstruction due to impaction of one or more gallstones within the gastrointestinal tract.1 This complication occurs most frequently in elderly patients. It develops in 0.3%-0.5% of patients with cholelithiasis and accounts for 1%-4% of mechanical intestinal obstructions.2,3 GI is frequently preceded by an initial episode of acute cholecystitis. The impacted gallstone causes mucosal ischemia and necrosis, which further erodes through the gallbladder wall and leads to fistula formation between the gallbladder and an adhered portion of the gastrointestinal tract, with subsequent gallstone passage.4,5 The majority of gallstones smaller than 2-2.5 cm will pass spontaneously through a normal gastrointestinal tract. Larger gallstones may suffer impaction and cause intestinal obstruction. The most common site of impaction is the terminal ileum and the ileocecal valve.1
The mainstay of treatment is surgical exploration, with enterolithotomy alone, or a one-stage procedure consisting of enterolithotomy, cholecystectomy and fistula repair in selected cases, as surgical options.6 Here we present a retrospective review of patients with GI diagnosis, treated during a 6-year period in three western academic centers in Mexico. The aim of this study was to describe the clinical manifestations, radiological and operative findings, surgical procedures and postoperative outcomes of patients with GI.
Patient population and study variables
We conducted a retrospective review of medical records for patients at three western Mexican academic institutions (Hospital Civil de Guadalajara Juan I. Menchaca, Guadalajara, Jalisco; Hospital Civil de Guadalajara Fray Antonio Alcalde, Guadalajara, Jalisco; Hospital General de Occidente, Zapopan, Jalisco) that underwent surgical treatment for GI between January 2015 and December 2020.
Patient data collection included demographics, preoperative comorbidities, clinical presentation, diagnostic workup, time interval from diagnosis to surgical treatment, surgical findings, details of the surgical procedure and postoperative complications.
The study was approved by the Committees of Human Research of each participant institution and was conducted in accordance with the principles of the Declaration of Helsinki.
Diagnostic and therapeutic approach
All patients were initially treated as a gastrointestinal obstruction, with fasting, volume resuscitation, and placement of a nasogastric tube in patients with severe bowel distension and vomiting. Diagnostic workup started with laboratory tests, plain abdominal radiographies, followed by ultrasound and computed tomography (CT) as needed.
All patients were surgically treated with an exploratory laparotomy and either enterolithotomy alone or a one-stage procedure of enterolithotomy plus cholecystectomy and fistula repair, according to surgeons´ decision.
Statistical analysis
Continuous data are presented as means ± standard deviation (SD) or medians (range). Qualitative variables are presented as frequencies and percentages for qualitative variables. Statistical analysis was performed using R software version 4.0.2 (Vienna, Austria).
During a six-year period, sixteen patients underwent surgical intervention for GI. Seventy five percent of patients were female and the overall median age was 55years (range 26-81). The most common comorbidity found in our patients was systemic arterial hypertension (56.2%), followed by diabetes mellitus (37.5%), and obesity (31.2%). Fifty percent and 37.5% of our patients had an American Society of Anesthesiologist (ASA) class III and class II physical status, respectively (Table 1).
Variables |
All patients (n = 16) |
Age (years) |
55 (26 – 81) |
Gender (females) |
12 (75%) |
Comorbidities |
|
Hypertension |
9 (56.2%) |
Diabetes mellitus |
6 (37.5%) |
Obesity |
5 (31.2%) |
CHF |
1 (6.2%) |
Hemolytic anemia |
1 (6.2%) |
ASA classification |
|
I |
2 (12.5%) |
II |
6 (37.5%) |
III |
8 (50%) |
Table 1 Demographic characteristics, comorbidities and ASA classification of 16 patients with gallstone ileus
Clinical, laboratory, and radiological findings
The median time for diagnosis from onset of symptoms was 6days (range 2-28days). Clinical presentation included abdominal pain in 15 patients (93.7%), followed by vomit in 13 patients (81.2%), abdominal distention and impossibility to pass feces and flatus in 11 patients (68.7%). Less common symptoms were fever in two patients and jaundice in one patient (Table 2).
Variables |
All patients (n = 16) |
Days from onset of symptoms to diagnosis |
6 (2 – 28) |
Clinical findings |
|
Abdominal pain |
15 (93.7%) |
Vomit |
13 (81.2%) |
Constipation |
11 (68.7%) |
Abdominal distension |
11 (68.7%) |
Fever |
2 (12.5%) |
Hemolytic anemia |
1 (6.2%) |
Jaundice |
1 (6.2%) |
Laboratory |
|
Electrolyte abnormalities |
14 (87.5%) |
Abnormal LFTs |
5 (31.2%) |
Radiological findings |
|
Radio-opaque gallstone |
11 (68.7%) |
Bowel distension |
10 (62.5%) |
Pneumobilia |
8 (50%) |
|
|
Table 2 GeneralClinical, laboratorial and radiological findings of 16 patients with gallstone ileus
Laboratory tests showed electrolyte imbalance in 14 patients (87.5%) and liver function tests abnormalities in five patients (31.2%). A correct preoperative diagnosis of GI was reached in 13 patients (81.2%); the remaining was diagnosed during surgery. The classical image signs of GI were visualized in 7 patients (43.7%) on plain abdominal radiograph (Figure 1), in six patients (37.5%) on ultrasound (Figure 2) (Figure 3), and in 13 patients (81.2%) on CT (Figure 4) (Figures 5a & b).
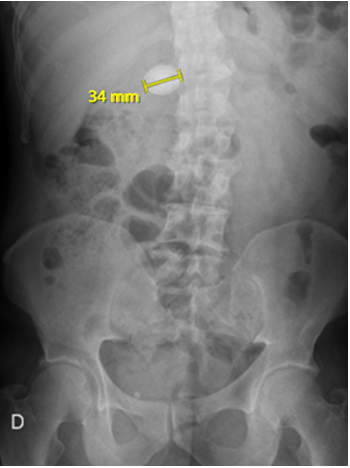
Figure 1 Plain abdominal radiograph showing a radio-opaque 34mm-image located in the right upper quadrant suggestive of a gallstone.
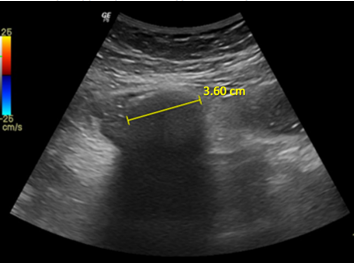
Figure 2 Abdominal ultrasound shows a hyperechoic oval-shaped image of 3.6 cm with acoustic shadow suggestive of a gallstone located in the right lower quadrant of the abdomen.
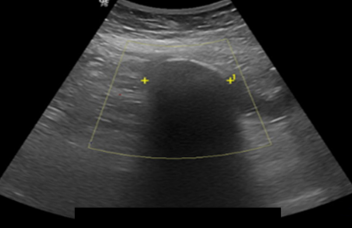
Figure 3 Abdominal ultrasound reveals an endoluminal hyperechoic round-shaped image with acoustic shadow located lateral to mesogastrium.
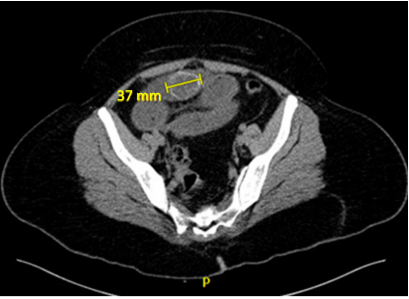
Figure 4 Computed tomography depicts an endoluminal oval-shaped image with calcium density, consistent with a migrated gallstone within the terminal ileum.
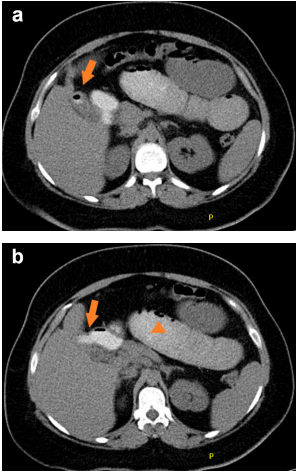
Figure 5A & 5B Oral contrast-enhanced computed tomography findings in a patient with gallstone ileus. a. Gas observed within the gallbladder (arrow) b. Communication between a non-distended gallbladder and the duodenum, where presence of oral contrast is observed in the site of the fistula (arrow), and fluid-filled dilated jejunal loops and intestinal pneumatosis (arrowhead).
Image findings included radio-opaque image suggestive of a gallstone in 11 patients (68.7%), (Figure 6) bowel distention in 10 patients (62.5%) (Figure 7), and pneumobilia in 8 patients (50%) (Figure 8), all classical signs of Rigler´s triad.7
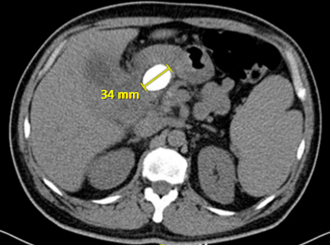
Figure 6 Computed tomography reveals a calcium density endoluminal foreign body of 34 mm, located in the topography of the duodenum.

Figure 7 Fluid-filled dilated intestinal loops and hydro-air level (arrowhead), intestinal pneumatosis (arrow), and an endoluminal round-shaped calcium-density image of 50 mm are seen.
One 80years-old female with gastric outlet obstruction syndrome was diagnosed through a gastroduodenoscopy where the gallstone was found in the second portion of duodenum. (Figures 9A & B) An endoscopic attempt to extract the stone failed, so she was surgically intervened. Table 3 shows the details of our study population (Table 3).
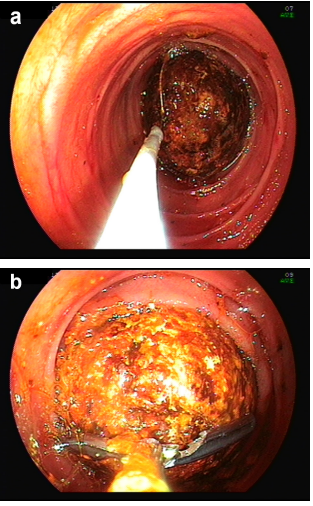
Figure 9 Endoscopic findings during a gastroduodenoscopy performed to a patient with Bouveret´s syndrome. a. Gallstone impacted within the 2nd portion of duodenum showing a failed attempt to extract it with a Roth net. b. A rat-tooth retrieval forceps.
Gender / age (years) |
Comorbidities |
ASA |
Onset of symptoms (days) |
Diagnostic method |
Surgical |
Site of obstruction |
Morbidity |
Clavien-Dindo |
M / 50 |
DM Hemolytic anemia |
II |
6 |
Plain abdominal radiograph, CT |
Enterolithotomy |
Stomach |
None |
1 |
F / 26 |
Obesity |
II |
8 |
US, CT |
Enterolithotomy |
Ileum |
Enterorraphy dehiscence |
3b |
F / 49 |
None |
II |
2 |
US, CT |
Enterolithotomy |
Ileum |
None |
1 |
F / 69 |
DM, SAH |
III |
2 |
US, CT |
Enterolithotomy + cholecystectomy + fistula closure |
Ileum |
Pneumonia |
2 |
M / 63 |
SAH, CHF |
III |
2 |
US |
Enterolithotomy + cholecystectomy + |
Jejunum |
Pleural effusion |
2 |
|
|
|
|
|
fistula closure |
|
|
|
F / 78 |
DM, SAH |
III |
4 |
Plain abdominal radiograph |
Enterolithotomy |
Ileum |
Pneumonia, |
5 |
F / 81 |
DM, SAH |
III |
10 |
Plain abdominal radiograph, CT |
Enterolithotomy + intestinal resection and anastomosis |
Ileum |
Pneumonia, pleural effusion, acute renal failure, SSI |
2 |
M / 72 |
SAH |
II |
4 |
Plain abdominal radiograph, CT |
Enterolithotomy |
Ileum |
Acute renal failure |
2 |
F / 49 |
Obesity |
I |
4 |
Plain abdominal radiograph, CT |
Enterolithotomy |
Ileum |
None |
1 |
M / 47 |
None |
I |
9 |
Plain abdominal radiograph, US, CT |
Enterolithotomy |
Ileum |
None |
1 |
F / 51 |
Obesity |
III |
12 |
US, Plain |
Enterolithotomy + |
Ileum |
Seroma |
2 |
|
|
|
|
abdominal radiograph |
cholecystectomy + fistula closure |
|
|
|
F / 59 |
SAH, Obesity |
III |
28 |
CT |
Enterolithotomy |
Ileum |
Pneumonia |
2 |
F / 48 |
SAH |
II |
16 |
CT |
Enterolithotomy |
Ileum |
Seroma |
1 |
F / 67 |
DM, SAH, |
III |
20 |
CT |
Enterolithotomy + cholecystectomy + fistula closure |
Duodenum |
Acute renal failure, |
2 |
F / 40 |
DM |
III |
3 |
CT |
Enterolithotomy + cholecystectomy + fistula closure |
Ileum |
Diabetic ketoacidosis |
2 |
F / 80 |
SAH |
II |
7 |
EGD |
Enterolithotomy |
Duodedum |
Enterorraphy dehiscence, death |
5 |
Table 3 Demographic characteristics, comorbidities, ASA classification, diagnostic method, surgical procedure, site of obstruction, postoperative morbidities and Clavien-Dindo classification of 16 patients with gallstone ileus
M, male; F, female; DM, diabetes mellitus; SAH, systemic arterial hypertension; CHF, congestive heart failure; CT, computed tomography; US, ultrasonography; EGD, esophagogastroduodenoscopy; SSI, surgical site infection
Operative findings
All patients underwent surgical treatment. Impacted gallstone was located in the terminal ileum in 12 patients (75%), in duodenum in two patients (12.5%), followed by stomach and jejunum, each in one patient (6.2%). The median number of intraluminal gallstones was 1 (range 1-6) with a median size of 3.6 cm (range 2-8cm). The site of bilioenteric fistula was documented during surgery in 14 patients (87.5%). Due to severe inflammation in the right upper quadrant, it could not be documented in the rest of them. Cholecystoduododenal fistula was the most common type (75%) of our patients, followed by cholecystogastric fistula (12.5%) (Table 3).
During exploratory laparotomy, enterotolithotomy alone was performed in 11 patients (68.7%); two of such enterolithotomies were performed in the duodenum followed by simple duodenorraphy, due to poor clinical conditions of the patients. In one patient the gallstone was extracted through a gastrotomy. An intestinal resection and anastomosis was needed to extract the stone and remove an ischemic ileum segment in one patient. In the remaining 12 patients the procedure was completed with enterotomy and transverse enterorraphy (Figure 10). A Meckel´s diverticulum was incidentally found in an 81years-old female but since it was not complicated, no surgical management was needed (Figure 11). One-stage-procedure was performed in 5 patients (31.2%). No patient was managed with a two-stage procedure. Median intraoperatory blood loss was 110ml (range 40-350), median surgical time was 100minutes (range 53-230), and median hospital stay was 7 days (range 1-17).
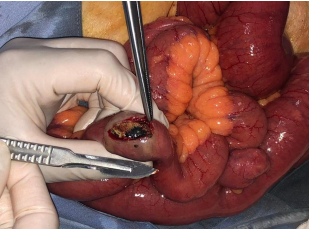
Figure 10 Surgical findings in a patient with gallstone ileus. Enterotomy performed over the site of the impacted gallstone in the terminal ileum.
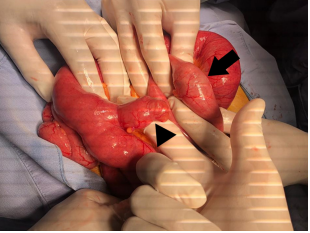
Figure 11 Surgical findings in patient with gallstone ileus. a. Segment of ileum at 60cm from the ileocecal valve with non-complicated Meckel´s diverticulum (arrowhead) and site of impacted gallstone in ileum, at 50 cm from the ileocecal valve (arrow).
Morbidity and mortality
The overall morbidity rate was 75% since complications occurred in 12 out of 16 patients. Twenty five percent of patients had pneumonia, 18.7% developed acute renal failure, 12.5% had a pleural effusion or atelectasia, and 12.5% showed signs of dehiscence of the duodenal enterorraphy performed during surgery. Sixty two percent of patients developed other complications including superficial surgical site infection, fluid sterile collection, mild acute pancreatitis, and poor glycemic control. Two patients (12.5%) died as a consequence of sepsis due to enterorraphy dehiscence. According to the Clavien-Dindo Classification.8, complications, 50% were classified as grade II, 31.25% as grade I, 12.5% as grade V, and 6.2% as grade IIIb. Mean follow-up was 291 days (range 4 to 1460). During this time, there were no cases of recurrent GI or other late biliary complications. Table 4 shows the treatment details and outcomes of our patients. (Table 4).
Variables |
All patients (n = 16) |
Correct preoperative diagnosis |
13(82.1%) |
Location of impacted gallstone |
|
Stomach |
1 (6.2%) |
Duodenum |
2 (12.5%) |
Ileum |
13 (81.2%) |
Number of intraluminal gallstones |
1 (1 – 6) |
Size of intraluminal gallstones (cm) |
3.6 (2 – 8) |
Location of bilioentérica fistula |
|
Cholecystogastric |
2 (12.5%) |
Cholecystoduodenal |
12 (75%) |
Not documented |
2 (12.5%) |
Surgical procedure |
|
Enterolithotomy |
11 (68.7%) |
Enterolithotomy + cholecystectomy + |
5 (31.2%) |
Additional surgical procedure |
|
Duodenotomy |
2 (12.5%) |
Gastrotomy |
1 (6.2%) |
Intestinal resection and anastomosis |
1 (6.2%) |
Intraoperative blood loss (ml) |
110 (40 – 350) |
Surgical time (min) |
100 (53 – 230) |
Early postoperative complications |
|
Pneumonia |
4 (25%) |
Acute renal failure |
3 (18.7%) |
Pleural effusion / atelectasia |
2 (12.5%) |
Dehiscence of enterorraphy |
2 (12.5%) |
Others |
10 (62.5%) |
Death |
2 (12.5%) |
Clavien-Dindo Classification |
|
Grade I |
5 (31.2%) |
Grade II |
8 (50%) |
Grade IIIb |
1 (6.2%) |
Grade V |
2 (12.5%) |
Hospital stay (days) |
7 (1 -17) |
Follow-up (days) |
291 (4 – 1460) |
|
|
Table 4 Treatment and outcomes of 16 patients with gallstone ileus
Gallstone ileus (GI) is a true mechanical obstruction caused by a biliary calculus that migrates from an inflamed gallbladder to the adjacent intestinal tract.5. Thomas Bartholin described the first case of GI en 1654, during a necropsy. In 1841, Bonnet presented the first case of duodenal obstruction in the duodenal bulb (Bouveret’s syndrome). In 1890, Courvoisier published the first 131 cases of GI; 125 of such patients were operated, with a mortality of 44%.9
GI is a rare complication of gallstone disease that most frequently occurs in elderly patients, with an occurrence of 0.3-0.5% in patients with cholecystolithiasis.2,3 This entity causes only 1% to 5%% of all cases of mechanical bowel obstructions, but may be responsible for up to 25% of cases of small bowel obstruction in patients older than 65 years, with a female preponderance.10-12
In the present series, the median age was 55 years, and 37.5% of our patients were 50years old or less. Elderly patients constitute the majority of cases with GI, but patients in the third and fourth decade of life have also been observed in recent series.6,13,14 In our series we only had one patient 26years old with GI.
Clinical presentation of gallstone ileus has not changed in a long time. The classic presentation is an older female patient with episodic subacute obstruction. There are three forms of presentation: acute, subacute, or chronic (Karewsky´s syndrome). This clinical presentation may be given depending on the site of obstruction and the size of the gallstone.15 Diagnosis of GI can be challenging due to several factors: the intermittency of the symptoms, the fact that signs and symptoms are nonspecific, the advanced age of the patients and their concomitant diseases.11,16 The median time to reach diagnosis from onset of symptoms was 6days (range 2-28 days). The majority of patients present 4 to 8 days after the onset of symptoms, which include crampy abdominal pain, nausea, and vomiting. Other signs and symptoms are jaundice (<15%), abdominal distension and fever.16 This is consistent with the clinical manifestations of our patients in whom we found abdominal pain, vomiting, abdominal distention, and impossibility to pass stools and gas in more than 60% of cases, fever in 12.5%, and jaundice in 1 patient (6.25%) only. We also had two patients with Bouveret’s syndrome and classical symptoms of gastric outlet obstruction (early satiety, epigastric pain, nausea, nonbilious vomiting, anorexia) but none with upper gastrointestinal bleeding caused by erosion of the duodenum by the impacted gallstone, as other authors have reported.16
Obstruction of the bowel usually occurs after the impaction of a gallstone at least 2.5cm in diameter. Clavien et al. reported the size of obstructing gallstone from 2 to 5cm.3 Nakao et al. found a range gallstone size of 2-10cm.14 In our patients the median size of gallstones was 3.6cm (range 2-8cm). Usually, a single intraluminal gallstone can be located during surgery.15 Cases of multiple gallstones have been reported in 3 to 40% of cases.3,17 Surgeons are encouraged to palpate and explore the whole bowel length in search for more than one gallstone, which could cause recurrent GI episodes.1,16 In our series, multiple gallstones were found and extracted in three patients, two gallstones in two patients, and six gallstones in one patient. No recurrent GI episodes were documented during follow-up.
The most common sites of gallstone impaction is the ileum (0%-89.5%), followed by the jejunum (0%-50%), stomach (0%-20%), duodenum (0%-10.5%), and colon (0%-8.1%).16,18 In our series, we found a similar frequency of gallstone impaction, as the majority was found in the ileum (81.2%), followed by the duodenum (12.5%) and the stomach in one case (6.2%).
Gallstone migration from the gallbladder to the gastrointestinal tract occurs more frequently through a cholecystoduodenal fistula, with rates in the range of 32.5%-96.5% of cases.16,19 In our patients the cholecystoduodenal fistula was the most common location site of gallstone migration (75%), followed by a cholecystogastric fistula (12.5%). Due to severe inflammation in the right upper abdominal quadrant, identification of fistula could not be achieved in the remaining 12.5% of cases. Other sites of bilioenteric fistula have been described at the right or transverse colon, jejunum, and even more rare locations such as duodeno-left hepatic biliary duct.5, 9, 20
Radiologic workup is crucial for the diagnosis of GI. The Rigler´s Triad7 of pneumobilia, ectopic radio-opaque gallstone and intestinal distension, is variably found on plain abdominal radiographs in 17-87% of cases.9, 21 Balthazar and Schechter described another sign consisting of the presence of two fluid-filled loops in the right upper quadrant: the medial one corresponding to the duodenal bulb and the lateral one to the gallbladder, due to the presence of air within this organ.22 Abdominal ultrasound can also provide useful information, which includes the presence of bilioenteric fistula, a gallstone impacted within the bowel, gastric distension as seen in Bouveret’s syndrome, and residual gallstones within the gallbladder or choledocholithiasis, being these two last findings the most valuable ones, since this would encourage the surgeon to consider cholecystectomy and even bile duct exploration during surgical treatment.9,18,21 Ultrasound is also considered highly sensitive for pneumobilia and ectopic gallstones, but in cases of complete bowel obstruction the exam can be technically difficult to perform, due to patient discomfort and intraluminal gas interposition.18 The combination of ultrasound and plain radiographs increases the sensitivity of GI diagnosis to 74%.18, 21,23
Contrast-enhanced abdominal CT represents the best radiologic method to diagnose GI, with 93% sensitivity and 100% specificity.24 Additional signs that can be found on abdominal CT are changes in the gallbladder wall suggestive of chronic cholecystitis, location of bilioenteric fistula and size and location of intraluminal gallstones.9 In our series, we found an ectopic radio-opaque gallstone in 68.75%, bowel distension in 62.5%, and pneumobilia in 50% of cases, with the combined diagnostic workup of plain radiographs, abdominal ultrasound, and CT. A correct preoperative diagnosis has been reported in other series between 30% and 75% of cases.16 In our patients we were able to make this correct preoperative diagnosis of GI in 13 patients (81.2%).
Surgery is the standard approach for gallstone ileus. Its main objective is to relieve the intestinal obstruction once hydro-electrolytic correction and hemodynamic stabilization have been achieved. Three possible procedures have been described: enterolithotomy alone, one stage surgery that consists of enterolithotomy plus cholecystectomy plus fistula repair, and two-stage surgery that involves enterolithotomy alone, with a second surgical event to repair the fistula and perform cholecystectomy. Enterolithotomy alone is the most commonly performed procedure.15,16 An enterotomy in the antimesenteric border over the offending gallstone is performed and transverse enterorraphy in a Heineke-Mikulicz fashion is recommended to avoid stenosis.2,3 This surgical approach was performed in 68.75% of our patients. One-stage surgery has been advocated for patients with hemodynamic stability and with low surgical risk (ASA I and II). This approach has the advantage of preventing recurrent GI and other late biliary complications associated to an unsolved cholecystolithiasis: cholecystitis, cholangitis, acute pancreatitis, choledocholithiasis and gallbladder carcinoma.16 We performed such one-stage approach in 31.25% of our patients. We treated 11 of our patients (68.7%) with enterolithotomy alone and after a mean follow-up of 291days, there were no cases of recurrent GI or other late biliary complications.
There have been conflicting results regarding the morbidity and mortality of the three different surgical approaches used to treat GI. Simple enterolithotomy has been associated with lower morbidity and mortality compared to the one-stage procedure according to some authors.10,25 Although other authors prefer the one-stage surgery, when patients in different surgical groups were comparable in terms of age, concomitant diseases and APACHE II score, operative morbidity and mortality rates have not been significantly different.3. Other studies have reported a higher morbidity among patients treated with the one-stage procedure, even when the ASA scores were similar for both groups of patients.25 Thus, the one-stage procedure should be performed in highly selected patients who have been adequately reanimated and have absolute indications for biliary surgery at presentation, such as acute cholecystitis, gallbladder necrosis or residual gallstones.3, 10,11, 14,26
Postoperative complications have been estimated in the range of 45% to 69%. The most common postoperative complications are surgical site infection, followed by acute renal failure, pneumonia, urinary tract infection and anastomotic leaks.3, 15,16,26-28 In our series, we report an overall morbidity rate of 75% (12 patients). This is rate is higher than those reported by other authors, but 50% of complications in our series corresponded to Clavien-Dindo I, which might be underestimated in many series. In our series, complications were documented in 60% of patients treated by enterolithotomy alone, and 100% of patients managed with a one-stage surgery. This might be related to a higher median age in the one-stage surgery group of patients (65 years, range 40-81, vs. 49 years, range 26-80). The ASA classification was also higher among patients in the one-stage surgery group, where 100% had an ASA score of III. More patients in the one-stage surgery group were affected by SAH (66% vs. 50%), DM (66% vs. 25%) and obesity (33.3% vs. 20%). Similar results have been reported by previous series.
Mortality rate ranges from 0% to 24%.12,15,25,27,29 Higher mortality rates have been associated to major proportion of elderly patients among those affected by GI, their concomitant diseases and age-related surgical complications.16 The one-stage surgical approach has been independently associated to mortality.12 When analyzed by surgical procedure, mortality rate is higher for the one-stage surgery group (0% - 15%) than for the enterolithotomy alone group (0% - 25%).12,15,25,29,30 When bowel resection is required due to vascular compromise at the site of gallstone impaction, mortality rates from 13% to 50% have been reported.12,30 In our series, one patient with a gallstone impacted in the ileum required resection and anastomosis. The patient developed pneumonia, pleural effusion, acute renal failure, and surgical site infection, but finally recovered.
The present study examined the diagnostic and therapeutic approach of patients with GI in three academic hospitals in the same city, over a 6-year period. The present study has several limitations. The retrospective design constitutes the main limitation. The second one is the reduced number of patients that resembles the low number of patients in most series and the low frequency of presentation of this clinical entity. Ideally, randomized controlled clinical trials would be needed to establish the best surgical approach, which could be difficult to perform in the clinical scenario.
Gallstone ileus is a rare cause of gastrointestinal obstruction, with female and elderly population preponderance, although younger patients are affected. A high clinical index of suspicion guides image modality selection, where CT is the most useful image study used. An adequate preoperative stabilization and optimization of comorbidities will allow a better outcome. Surgical relief of gastrointestinal obstruction is the cornerstone of treatment. Enterolithotomy alone is the most frequent surgical approach and has a lower morbidity rate. Indications for a one-stage surgical approach remain to be established.
None.
The authors declare that they have no conflicts of interest.
Design of the study: Itzé Aguirre-Olmedo
Data acquisition and analysis and interpretation of data: Itzé Aguirre-Olmedo, Santiago Rea-Alvarez del Castillo, Carlos M. Nuño-Guzmán, Alberto Briceño-Fuentes, Román I. García-González, M Carmen Torres-González, Felipe Ferrari-Ulloa, A. Rebecca Juárez-González.
Drafting of the manuscript: Itzé Aguirre-Olmedo, Santiago Rea-Álvarez-del-Castillo, Carlos M. Nuño-Guzmán, Román I. García-González, M Carmen Torres-González, Felipe Ferrari-Ulloa.
Manuscript writing: Itzé Aguirre-Olmedo, Santiago Rea-Álvarez-del-Castillo, Carlos M. Nuño-Guzmán.
None.

©2022 Aguirre-Olmedo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.