eISSN: 2373-6372


Clinical Paper Volume 11 Issue 1
1Department of Thoracic and General Surgery, Arya Hospital, Iran
2Department of Gastroenterology, Arya and Golsar Hospitals, Iran
3Department of vascular surgery, Arya Hospital, Iran
4Department of Internal Medicine, Inflammatory Lung Diseases Research Center, Iran
Correspondence: Yousha Pourahmadi, Resident of general surgery, and Inflammatory Lung Diseases Research Center, Department of Internal Medicine, Razi Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
Received: November 30, 2019 | Published: January 23, 2020
Citation: Aghajanzadeh M, Shafaghi A, Hemmati H, et al. Esophageal diverticulum fistula to the right lung lower lobe presented with massive upper gastrointestinal bleeding: a rare case. Gastroenterol Hepatol Open Access. 2020;11(1):29-34 DOI: 10.15406/ghoa.2020.11.00409
Background – Esophageal respiratory fistulas are abnormal connections between the esophagus and the respiratory system. Two types of these fistulae may be present as congenital or acquired. Most common sites of acquired esophageal pulmonary fistula are between esophageal tracheal and esophageal bronchial tree and the most common causes are infections or malignant neoplasms. An esophageal pulmonary fistula due to diverticula with presentation of hematemesis is extremely rare.
Case presentation: This case concerns a man aged 67years with a lower third of esophageal diverticula and pulmonary fistula presented with abrupt-onset of cough and massive hematemesis. Imaging study findings suggested a fistula between the lower third of the esophagus and the lower lobe of right lung. Fibro-optic-esophagoscopy was performed which showed massive clots in the lumen of esophagus, the diagnosis was an acquired esophageal pulmonary fistula. CT-angiogram of aorta and pulmonary artery revealed pulmonary artery to lower esophagus fistula. The patient underwent right lung lower lobectomy partial esophageal resection. Three days postoperatively an esophagus–pleural fistula developed. After putting a self-expandable metallic stent, leakage was closed. Patient discharged 15 days after operation with good condition. In two months postoperative follow-up, the patient was still in good condition.
Conclusions: Esophageal respiratory fistulae with massive hematemesis must be suspected, particularly in a patient with pneumonia in the lower lobs and resistant to antibiotic treatment. Esophageal pulmonary fistulae are diagnoses by means of radiological imaging or esophagoscopy. Esophageal respiratory fistulae can be acute and life-threatening so prompt treatment with endoscopic placement of covered stent or via surgery is needed.
Keywords: esophageal pulmonary fistula, hematemesis, esophageal diverticula, esophageal stent
ED, esophageal diverticula; EED, epiphrenic esophageal diverticula; COPD, chronic obstructive pulmonary disease
Esophageal diverticula (ED) is rare disorder of esophagus that have a prevalence of 0.015–2%.1–3 Most esophageal diverticulas are acquired which present in older adults,5 the average age of patients at the time of diagnosis is 60–70 years old,1,2,4–6 and there is a male–female ratio of around 2:1.1,2,3,6
Epiphrenic esophageal diverticula (EED) is located in 10cm of the gastro-esophageal junction and is responsible for about 15% of all esophageal diverticula.The majority of EED are false diverticula which contain the mucosal and submucosal layers without the muscularis propria.1-4,6,7 EED more commonly occurs on the right side because heart and aorta inhibit the growth of diverticula on the left side.2-4,7
Esophageal Diverticula (ED) is an uncommon disease which is classified in to three types according to anatomical place: cervical, thoracic and epiphrenic. Pathogenesis of these diverticula is divided to pulsion and traction, and according to morphology they are true or false. ED usually happens in the middle and lower third of the thoracic esophagus.1–3
Peribronchial diverticula usually occurs due to mediastinal inflammatory diseases such as histoplasmosis or tuberculosis. A true diverticulum is formed as a result of full thickness esophageal wall pinching due to desmoplastic reactions.1–3,5 These kinds of diverticula often are established in the right side possibly due to nearness of the lymph nodes in this area and the right anterior wall of the esophagus in old people.5,6,8 The majority of epipherinic ED are associated with motility disorders so that esophageal myotomy is needed during diverticulectomy.5–9,10 Esophageal myotomy is a surgical procedure of cutting away some of the outer muscle layers of lower esophagus for better passage of liquids and food from the esophagus into the stomach and preventing recurrence of diverticulum. It can be done via Laparoscopy open surgery or endoscopy.10 Diveticulectomy is surgical removal of diverticulum and repairing the defect with suture.11
Epiphrenic Esophageal Diverticula (EED) symptoms are mostly regurgitation and intermittent dysphagia [5,8,9,] while about 80% of patients with ED have a few symptoms or are asymptomatic.5,6,10,12 One of the very rare and serious ED complications is upper gastrointestinal bleeding and pulmonary aspiration.1,5–7,13 Imaging evaluation of ED includes chest X-ray, esophagoscopy and barium esophagogram. Historically the best approach for treatment of ED was surgery, however recently interventional endoscopy is the preferred management.14 Management of ED with fistula and bleeding includes a hemostatic clip placement over thermal coagulation and endoscopic esophageal stenting which is the preferred approach.14 Esophageal stenting is a safe approach and results in fistula healing, pulmonary sepsis improvement, and improved nutritional status.14,15
Laparoscopic diverticulectomy, thoracoscopic procedures and myomectomy are available surgical procedures.14 In this report we present a case of EED with fistula to right lung lower lobe presented with massive hematemesis. Hematemesis refers to bloody vomiting that usually indicates upper gastrointestinal tract hemorrhage.16 Urgent endoscopic therapy didn’t stop the bleeding so we performed thoracotomy, lobectomy and partial diverticulectomy to stop bleeding which was life-saving. This case is the second reported ED to a pulmonary lobe and the first case was EED fistula to the left lung lower lobe.17,18
A 67-years old man was admitted to our emergency room with episodes of melena, cough and massive hematemesis. He mentioned a history of pulmonary problem as COPD, lower third of esophageal diverticula and anemia. Chronic obstructive pulmonary disease (COPD) is a progressive chronic inflammatory lung disease related to long-term exposure to cigarette, pipe, or other types of tobacco that causes shortness of breath.19 He mentioned daily use of naproxen and pantoprazole for arthritic and epigastric pain respectively, and was heavy smoker.
On admission his blood pressure was 110/60 mmHg, heart rate 98 beats per minute and there was orthostatic hypotension on examination. Laboratory tests revealed a hemoglobin level of 7.8/dL (normal range 14.0–18.0g/dL), hematocrit of 22% (normal range 40.0–52.0%), blood urea nitrogen of 35mg/dL (normal range 7–20mg/dL) and creatinine 1.8ml/dL (normal range 0.5–1.2ml/dL). Initial management in the emergency room was hydration with normal saline boluses and continuous infusion of pantoprazole 80mg/h. The patient was moved to the intensive care unit, since he had three additional episodes of hematemesis with cough in the emergency room. Hemoglobin dropped to 6.8g/dL with a hematocrit of 18.2%. His blood pressure fell by 60/30mmHg.
We put him on a peripheral dopamine infusion for blood pressure support and ordered four units of packed red blood cells transfusion. Considering the past medical history, the suspected causes of massive upper gastrointestinal bleeding included, peptic ulceration, ruptured esophageal varice, mucosal tear of esophagus, diverticula bleeding and less likely esophageal diverticula with pulmonary or aorta fistula.
After patient’s stabilization, A chest CT-scan with IV contrast was performed. CT-scan showed a cavity in the right lung lower lobe which was connected to esophagus with leakage of contrast in the lumen (Figures 1 & 2). Urgent upper endoscopy was performed 12 hours after admission that revealed a huge clotted blood in the left-sided distal portion of esophagus. Blood clot was visualized and it was washed off and removed after irrigation, while an actively oozing blood vessel was the source of bleeding. Two days later, three episodes of hematemesis happened again so that the patient underwent re-endoscopy in which there was an orifice in the right side of esophagus from a cavity. At this time the diagnosis was fistula of esophagus diverticula to aorta, pulmonary parenchyma or heart chambers.
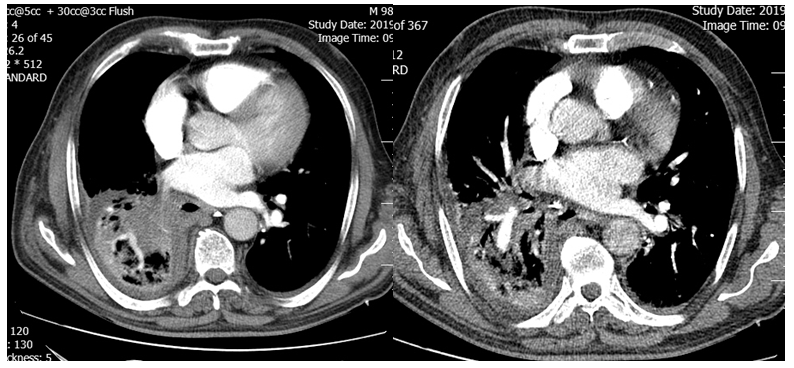
Figure 1 CT-scan with IV contrast shows a cavity in the right lung lower lobe which seemed to be connected to esophagus considering leakage of contrast in the lumen.
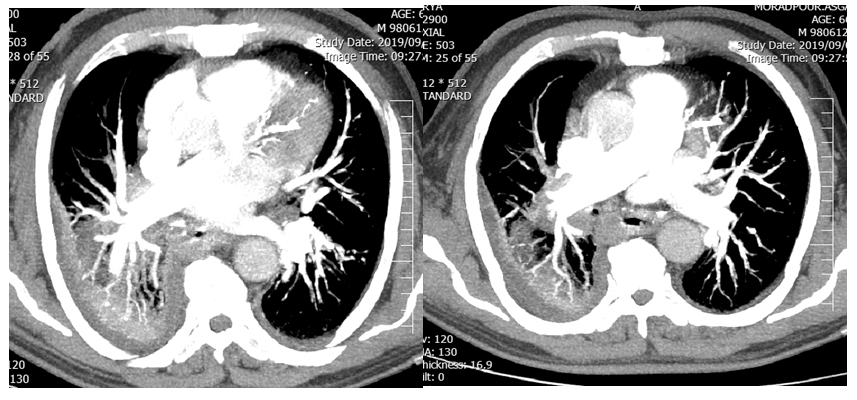
Figure 2 CT Angiography of pulmonary artery shows branch of pulmonary artery in the cavity, contrast around and in the lumen of esophagus.
We treated fistula by implanting a covered self-expandable metallic stent above the lower esophageal sphincter. Overnight, the patient had three additional episodes of hematemesis. At this point we were suspicious of pulmonary or aorta fistula to diverticula so that we performed a CT-angiograph of aorta and pulmonary artery. Aorta was intact, but fistula between diverticula and pulmonary artery was present (Figure 2). The patient underwent right postero-lateral thoracotomy; right lower lobe was severely adhesive to the mediastinum and esophagus. After pneumolysis, right lower lobectomy was performed and huge diverticula was present as a cavity, because of sever adhesion of diverticula to mediastinum partial diverticulectomy was performed and remnant diverticula was closed.
The following day, he was hemodynamically stable and off vasopressors, also his hemoglobin and hematocrit were 8.5g/dL and 24% respectively. Vital signs remained stable. Four days after operation, an esophageal barium study was performed and an esophago-pleural fistula was present (Figures 3 & 4). Fistula was closed using endoscopic esophageal stenting (Figure 5).20,21 Oral diet was started without any complications. He was discharged three days after the endoscopy procedure with 15 days total admission time. On outpatient follow-up one month after discharge, he was symptom free. A barium esophageal study was ordered to further evaluation of the stent location, which was right and the patient felt well after one month. The patient was asymptomatic with no recurrent diverticula and hematemesis at 3 months follow-up.
Lower esophageal diverticula are usually associated with motility disorders.1–3 The mechanism of EED formation is mostly secondary to pulsion forces associated with functional or mechanical obstruction or esophageal dysmotility. Esophageal wall is weaker in this portion which can produce mucosal herniation.2–5 Symptoms of ED are mostly intermittent dysphagia and regurgitation although, as our patient, many patients have a few symptoms or are asymptomatic. Other ED symptoms are dysphagia, belching, postural regurgitation, heartburn, retrosternal pain, and epigastric pain. Pulmonary complications ranges from nocturnal cough to life-threatening aspiration.
The most common cancer associated with ED, is squamous cell carcinoma which is a rare complication.15,22 One of the very rare and serious ED complications are Upper gastrointestinal bleeding.23,24 In review of literatures there are few reports [5-7] but esophagus to pulmonary parenchymal fistula with gastero-intestinal bleeding is extremely rare that our case is second esophagus to pulmonary parenchymal fistula reported case.17 There are two reported cases of fistula between esophagus and atrium and aorta that extremely are rare.
Diagnostic evaluation of ED includes chest X-ray, esophagoscopy and barium esophagogram.25,26 Historically the best approach for treatment of ED was surgery, however recently interventional endoscopy is the preferred approach.27,28 Elective surgical procedures include: laparoscopic diverticulectomy, thoracoscopy, thoracotomy, myomectomy, or anti-reflux procedure. In some cases of ED surgical evaluation are not necessary but some procedures are effective and hemostasis is achieved endoscopically.
Previously, some reports suggested that in a bleeding esophageal diverticulum, endoscopic approach should be considered as first-line treatment. Surgical procedures, closure by clipping, and metallic or silicone stents are current options. In our case stent couldn’t stop the bleeding, so that we performed thoracotomy and right lower lobectomy and partial resection of diverticula.
We describe a patient in whom a diverticulum communicated with the right lower lobe of the lung, and this fistula formation between an ED and the respiratory parenchyma leads to gastrointestinal tract bleeding which is a rare condition and optimal surgical treatment has not been reported. There is only one previous report of a Large Epiphrenic Esophageal Diverticulum Communicating with the left lower lobe17 in which they could not proceed with left lower lobectomy and myotomy due to the patient’s poor lung function, which was performing the reinforcement suture for the stapling line.17 We performed lobectomy without myotomy because we couldn’t find the esophagus due to sever adhesion. In that case the postoperative course was uneventful,29 but in our case fistula of esophagus to pleura was developed and which was managed with esophageal stenting. Patient discharged on day 15 postoperatively and in two months follow-up his condition was good.30
Esophageal respiratory fistulae with massive hematemesis must be suspected, particularly in a patient with pneumonia in the lower lobs which is resistant to antibiotics. Esophageal respiratory fistulae are diagnosed by imaging evaluation or esophagoscopy. Esophageal respiratory fistulae are acute, life-threatening conditions and treatment includes endoscopic stenting or surgery. Early detection and proper treatment are essential for symptom relief and survival.
The authors would like to thank Mr. Shahab Shahrabadi and shima Illdarii for editing of this paper.
Author declares that there are no Conflicts of interest.

©2020 Aghajanzadeh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.