eISSN: 2373-6372


Mini Review Volume 5 Issue 4
Department of Medical sciences, University of Sulaimaniyah, Iraq
Correspondence: Mohamed Alshekhani, MB ChB, CABM, FRCP-L, European Board Gastroenterology &Hepatology(EBGH), Kurdistan center for GEH; Faculty of Medical sciences, School of Medicine; University of Sulaimaniyah, Sulaimaniyah, Iraqi Kurdistan, Iraq
Received: August 02, 2016 | Published: October 21, 2016
Citation: Alshekhani M (2016) Endoscopic Rubber Band Ligation of Internal Hemorrhoids: Turning Hemorrhoidal Management from Surgery into an Office-Based Gastroenterology Endoscopic Practice. Gastroenterol Hepatol Open Access 5(4): 00150. DOI: 10.15406/ghoa.2016.05.00150
Hemorrhoids are laxed prolapsed anorectal fibrovasular cushions that cause symptoms when they prolapse excessively specially when they are traumatized by hard faeces causing bleeding. They are very common affecting up to 50% of the population especially elderly. Hemmorrhoids needs management when they become symptomatic especially when they bleed. Endoscopic rubber band ligation is increasing being recommended as the fist and best effective office-based out-patient treatment for symptomatic hemorrhoids, since other office-based treatment options and surgical approaches are more expensive, painful& associated with more complications.
Hemorrhoids are prolapsed lax fibrovascular cushions with the internal hemorrhoids (IH) being proximal to the dentate line, while the external hemorrhoidal cushions are distal to it. The anal submucosa forms a discontinuous layer of thickened tissue, creating “cushions” found in the left lateral, right anterior, right posterior positions, receiving their blood supply from the superior hemorrhoidal artery & branches of the middle hemorrhoidal arteries; with some communication with the inferior hemorrhoidal arteries. The venous drainage is provided by the superior, middle, inferior hemorrhoidal vessels, allowing for communication between the portal/ systemic circulations & form direct arteriovenous communications within the cushions, so hemorrhoidal bleeding is arterial in nature rather than venous. With time & aging, starting from 2nd -3rd decade, the cushions deteriorate or weaken, leading to distal displacement, venous distention, erosion, bleeding, thrombosis & prolapse. The cushions play important role in maintenance of rectal continence. Internal hemmoroides are graded in to four grades according to the degree of their prolapse through the anal canal & their reducibility, spontaneous or manual, while external hemmoroids are not classified. Pathophysiology of hemorrhoids include weakness of supporting tissue of the anal cushions, its downward displacement, causing venous dilation & prolapse with abnormal distention of the arteriovenous anastomoses within the cushions & abnormal dilatation of the veins of the internal hemorrhoidal venous plexus. Contributing factors include; Lack of dietary fiber, Chronic straining & spending excess time on the commode, Constipation, Diarrhea, Pregnancy, Sedentary lifestyle & Family history. Mostanorectal symptoms will often assumed to be due to hemmorrhoids, so it is always important to determine whether the symptoms are really due to hemmorrhoids, some other ano-colorectal problems, or a combination a of all. Up to 50% of rectal bleeding initially attributed to hemorrhoids turned out to have a different diagnosis after endoscopic evaluation including Colorectal Cancer(CRC).The majority of symptoms arise from enlarged IH, with bleeding being the most common presenting symptom, when the IH prolapse through the anal canal, becomes traumatized & friable, leading to bleeding. Hemorrhoids are AV plexuses, so the bleeding is typically bright red in color, not mixed with stool, can drip out & exacerbated by straining. Blood that is darker in color suggests other, more proximal sources. Bleeding Hemorrhoids typically do not cause a positive Hemoccult test by themselves. IH are covered with columnar mucosa, leading to mucous deposition on the perianal skin, itching / perineal irritation. The prolapsing tissue can impede the anal verge to “seal,” so causing fecal soiling. IH proximal to the dentate line is covered by relatively insensate mucosa, so they are typically not painful & rarely thrombose & if pain, we should look for coexistent complicating issues; such as anal fissures, Solitary Rectal Ulcer Syndrome (SRUS), Inflammatory Bowel disease (IBD), CRC, pelvic floor dysfunction, internal sphincter spasm, pelvic dyssynergia, proctalgia fugax, etc. External hemorrhoids are typically asymptomatic& pain usually results from thrombosed external hemorrhoids, as an acutely painful perianal swelling.1
Management of hemorrhoids includes medical, office-based endoscopic interventions & surgery. Medical management including increasing fiber intake to prevent constipation, avoiding prolonged straining, laxatives & use of vasoactive local soothing agents, should be tried in all patients and can provide symptomatic relief & prevent recurrence.
Office-based hemmotoidal interventions include hemmoroidal coagulation (using sclerotherapy, infrared, bipolar, heater probe, cryotherapy & direct currents) & endoscopic rubber band ligation using various office-based instruments or more effectively using flexible sigmoidoscopy for that purpose, frequently done in the retroflexed position,2 but can be done also by the forward view, since all the other non - RBL office-based hemmorrhoidal interventions are done in the forward view3 and the retroflextion in the rectum can cause pain, sometimes dislodgment of the RB- holding cap from the endoscope, can cause flattening of internal hemorrhoids and there are reports of rectal perforation using this approach.4–6 The flexible endoscopic RBL has the advantage of excluding other potential causes of hematochezia during the same session. The advantage of endoscopic RBL is that it can be applied for most grades of internal hemmoroides, sometimes even for grade 4.1,2 The only device specifically marketed for endoscopic band ligation of hemorrhoids is the Stiegmann-Goff Bandito Endoscopic Hemorrhoidal Ligator (ConMed Corp, Utica, NY), which fits on a 13- to 15-mm endoscope. Standard endoscopic variceal band ligation devices have been used as well. Rubber band ligation (RBL) is highly effective and the most commonly performed nonsurgical procedure in the treatment of hemorrhoids; used in up to 80% of treated patients.7 ASCRS guidelines, recommends RBL superior to injection sclerotherapy or infrared coagulation (IRC) for grades I, II, and III hemorrhoids.8 RBL is generally a simple, inexpensive procedure with many devices and ways of applying them.9 & performed with either a disposable suction device or a forceps ligator.10 There are also ligation techniques applied via the flexible endoscope that have demonstrated better visibility and comparable results.11,12 There are also a number of devices that are used through ananoscope or proctoscope as well as a “touch” method with bands placed without visualization by using a hand-held, disposable suction device.13
Surgery include Lord’s anal dilation, classical incisional surgery, stapled hemmoroidopexy & ultrasound-guided haemmorhoidal arteries ligation (HAL). Hemmoroidal surgery is so distressing to the patients that Senagore stated“ although few people have died of hemorrhoidal disease, many patients who have undergone certain hemorrhoid therapies wish they had died,”.1
A recent editorial comment on a research article published in the Lancet comparing HAL with RBL stated that evaluation of patient-reported dissatisfaction at 12 months revealed no difference between RBL & HAL, suggesting that multiple RBL had similar effectiveness than did HAL from the patients’ perspectives. Surprisingly, HAL was associated with increased pain & a persistent reduction in EQ-5D compared with RBL, contrary to the widely held belief that it represents a painless approach to management of haemorrhoids & Costs were also higher. RBL is an effective procedure and can be performed with either flexible or rigid endoscopes. Although it is easier to do multiple ligations with flexible endoscopes, discomfort and cost are reportedly higher. Suction band ligation was noted to be superior to forceps ligation with respect to pain and intraprocedure bleeding .In a study of 45 patients with chronic rectal bleeding secondary to second- and third-degree internal hemorrhoids randomized to RBL or bipolar coagulation therapy, success was higher with RBL with a similar safety profile. Recurrent symptoms were similar at 1 year. Experts caution against RBL of internal hemorrhoids in sedated patients because significant pain caused by errant band placement too close to or below the dentate line can occur. Usually, no more than 3 hemorrhoidal groups are banded in 1 session, although some experts advocate placing only 1 band at a time to minimize symptoms. Hemorrhoidal disease requiring the placement of 4 or more bands was associated with a trend toward higher failure rates and a greater need for subsequent operative hemorrhoidectomy (Figure 1-5).14,15

Figure 1 Rubber band ligator applied around a pile column by a video colonoscope using the forward view.
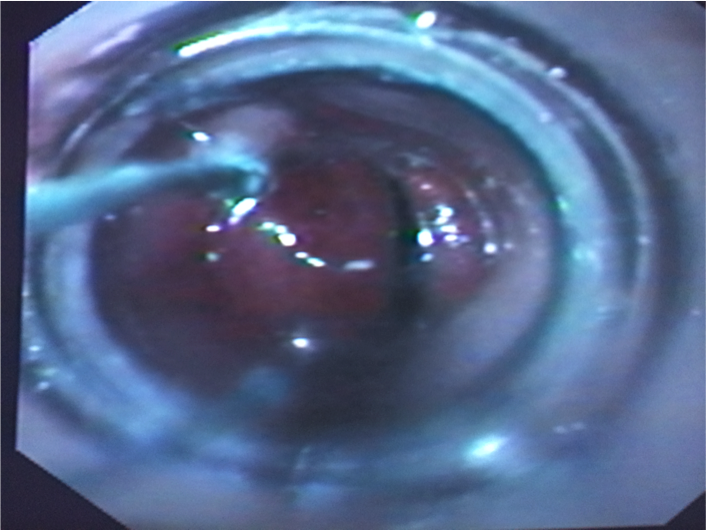
Figure 2 A black elastic rubber band ligator just applied on a pile column by a video colonoscope using the forward approach.
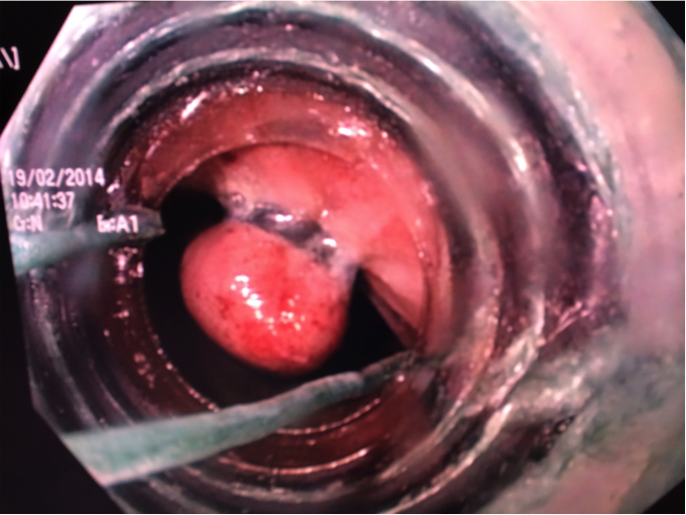
Figure 3 A white elastic rubber band ligator just applied on a pile column by a video colonoscope using the forward approach.
None.
The authors declare no conflicts of interest.
None.

©2016 Alshekhani. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.