eISSN: 2373-6372


Case Report Volume 4 Issue 3
Department of general surgery and department of pathological anatomy and cytology, Tunisia
Correspondence: Zaafouri Haithem, Department of general surgery and department of pathological anatomy and cytology, Habib Thameur hospital, 8 Ali Ben Ayed Street's, Monftfleury 1008, Tunis, Tunisia, Tel 21697348839
Received: December 15, 2015 | Published: March 23, 2016
Citation: Haithem Z, Mourad BB, Nizar K, Wafa K, Ahmed B et al. (2016) Colonic Tuberculosis. Gastroenterol Hepatol Open Access 4(3): 00103. DOI: 10.15406/ghoa.2016.04.00103
Tuberculosis is endemic in Tunisia. One-third of the world’s population is infected with tuberculosis (TB), with intestinal TB representing the sixth most common presentation of extra-pulmonary TB [1]. The diagnosis of intestinal TB is a challenge for physicians due to its diverse clinical manifestations that mimic other infectious, autoimmune, and tumor disorders, and is thus rarely considered as the causative agent of disease. Therefore, a high index of suspicion is essential to reach the correct diagnosis.
We report 3 cases of colonic tuberculosis which illustrate the variety of background circumstances and clinical manifestations that it may comprise.
Case n°1
We present a 45-year-old male with medical history of pleural tuberculosis for which he was treated with rifampicin, isoniazid, ethambutol and pyrazinamide since 3 weeks. He was admitted to the general surgery department for a small bowel obstruction with abdominal pain, vomiting and abdominal distension.
Abdominal examination revealed a diffuse distension with loud borborygmi and a tender left flank. The rectum was empty. Abdominal x-ray in up-right position showed fluid levels in the bowel. Biological investigations revealed a white cell count of 12700/mm3.
CT scan with contrast revealed a segmental thickening of the last ileal loops, distended small bowel loops without a detectable transition point, a 2 cm mesenteric mass associated with many mesenteric lymph nodes and magma of ileal loops some of which were contiguous to the sigmoid colon in the pelvis (Figure 1).
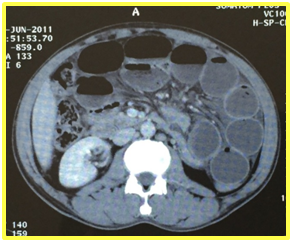
Figure1: A CT scan with contrast revealed a segmental thickening of the last ileal loops and distended small bowel loops without a detectable transition point.
A naso-gastric tube was placed on suction. There was no clinical improvement and surgical intervention was immediately prepared: the bowel obstruction was related to a mesenteric mass at which the small bowel and sigmoid colon were clustered and contiguous with dilation of the small bowel upstream. We performed a resection of the small bowel and sigmoid colon with the mesenteric mass. Pathological examination of the surgical specimen found a colonic tuberculosis fistulized in the mesentery (Figure 2).
He had an uneventful postoperative recovery and was discharged home with anti-TB medications. He remains asymptomatic 6 months following treatment with resolution of his symptoms.
Case n°2
A 21-year-old female was operated for an acute bowel obstruction related to a stenosis of the last ileal loop for which she had an ileo-cecal resection. Histological examination confirmed the diagnosis of ileo-cecal tuberculosis. She had a satisfactory evolution and was discharged. At 1 year follow-up she is doing well and has finished his course of anti-TB treatment.
Case n°3
An 18-year-old female presented with an intermittent diarrhea associated with peripheral and profound polyadenopathy. She had a colonoscopy with colonic and ileal biopsies. The mucosa of the left colon showed a pseudo-nodular appearance and was widely ulcerated in places. Anatomopathological examination found colonic tuberculosis. A treatment with anti-TB drugs was initiated and the outcome was uneventful [1].
Gastrointestinal tuberculosis is a quite common disease in our country, despite its prevention. Clinicians need to have gastrointestinal tuberculosis in their top diagnosis when dealing with patients with chronic gastrointestinal symptoms who are HIV-positive or coming from countries of high prevalence of TB. The signs and symptoms of intestinal TB are usually non-specific and diagnostic tests are sometime non-sensitive. A high level of evidence is required for an adequate diagnosis. Conservative management is successful in the majority of cases.

©2016 Haithem, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.