eISSN: 2373-6372


Case Report Volume 8 Issue 2
1Intensive care unit, Hassan I Hospital, Morocco
2Department of anaesthesiology and critical care, Ibn sina University Hospital, Morocco
3Department of gastroenterology, Ibn sina University Hospital, Morocco
Correspondence: Youssef Motiaa, MD, Intensive care unit, Hassan I Hospital, Tiznit Morocco Morocco, Tel (+212) 0671195295
Received: August 26, 2017 | Published: December 14, 2017
Citation: Motiaa Y, abdouni A, Rais S, Es-sadiki S, Ouassou Z (2017) Acute Colonic Pseudo-Obstruction Associated with Parkinson’s Disease. Gastroenterol Hepatol Open Access 8(2): 00277. DOI: 10.15406/ghoa.2017.08.00277
Acute colonic pseudo-obstruction (ACPO) or Ogilvie’s syndrome is defined as a massive dilation of the colon in absence of any mechanical obstruction. The majority of patients are midde-aged or elderly. The diagnosis of ACPO is based on Clinical presentation and excluding mechanical obstruction by imaging. Rapid diagnosis is the key, and institution of conservative measures often will lead to resolution. Delays in diagnosis can lead to fatal complications requiring a surgical treatment and increasing mortality. The management of Ogilvie’s syndrome is not codified. In this article, we report a case of ACPO in a 42years old patient with Parkinson’s disease and we discuss therapeutic approaches of Ogilvie’s syndrome.
Keywords: acute colonic pseudo-obstruction, parkinson’s disease, conservative treatment
Acute colonic pseudo-obstruction (ACPO) is defined as a massive dilation of the colon with obstructive symptoms, in the absence of mechanical obstruction.1 The incidence of ACPO is not known, and its pathophysiology in not clear; it is associated with imbalanced extrinsic autonomic innervation of gastrointestinal tract.1,2 Many conditions are associated with ACPO: medical or surgical causes and some medications. ACPO is characterized by abdominal distension, pain, nausea and/or vomiting.1,3 Delays in diagnosis or misdiagnosis can lead to mural ischemia; perforation and peritonitis requiring emergency laparotomy associated to high mortality. The treatment of ACPO is not consensual; it is based on conservative measures whilst surgical treatment is indicated for management of complications.
A 42years-old man, diagnosed with Parkinson’s disease one year earlier, on Levodopa / benserazide 250mg three times a day. He had no history of previous abdominal surgery. He was admitted into the emergency department for nausea, vomiting and generalized abdominal pain for a week. Physical examination revealed a distended and tympanitic abdomen. Bowel sounds were absent. Neurologic examination revealed Major akineto-rigid syndrome, no oculomotor or cognitive abnormality was noted. The patient was afebrile, conscious, blood pressure was 100/63mmHg, Harte rate was 90beat per min (bpm) and oxygen saturation rate was 97%.
Laboratory investigation revealed white blood cells (WBCs) 8.68 x 109/L; hemoglobin 14.8g/dl; aspartate aminotransferase (AST) 29IU/L, alanine aminotransferase (ALT) 19IU/L, total bilirubin 3.2mg/dl, direct bilirubin 0.5mg/dl, urea 0.54g/l, creatinine 8.8mg/dl, potassium 3mmol/L, chloride 98mmol/l and calcium 2.19 mmol/l. C-reactive protein 167.1mg/l. Abdominal computed tomography (CT) with intravenous contrast showed dilated bowel with no evidence of mechanical obstruction or Pneumoperitoneum (Figures 1a & 1b). The distension involved mostly the colon with caecum diameter of 6.79cm with pneumatosis intestinalis (Figures 2a & 2b).

A) Dilatation of all part of the colon.

B) Absence of pneumoperitoneum and mechanical obstruction.
Figure 1 N=57; Epidemiological distribution of the pathological fractures, traumatic fractures, and nonunion.
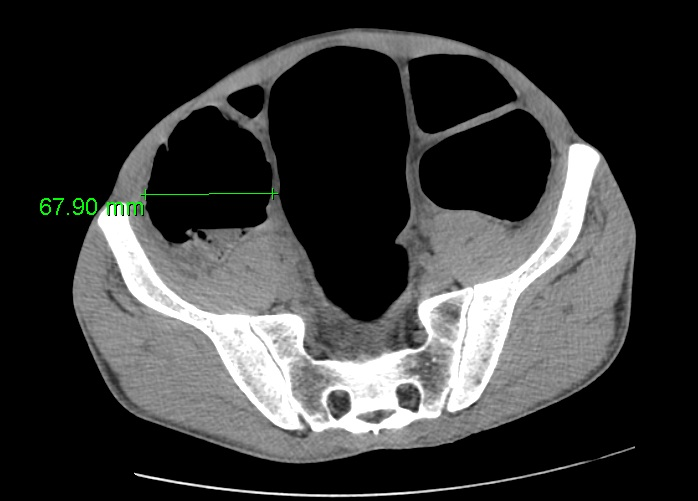
A) Cecum diameter at 6,79 cm.

B) Pneumatosis intestinalis
Figure 2 Impact of acute colonic pseudo-osbtruction.
Acute pseudo-obstruction of the colon was diagnosed and the patient was admitted to intensive care unit for monitoring, hydration and correction of electrolytes disturbances. Enteral feed was stopped; nasogastric decompression and rectal tube placement allowed a Subsidence of abdominal distension. Levodopa/benserazide was resumed after 3days. The patient was discharged to medical ward 3days later, after electrolytes were replaced and symptoms resolved.
Acute Colonic Pseudo-obstruction or Ogilvie’s Syndrome consists of dilatation of part or all of the colon and rectum without intrinsic obstruction or extrinsic inflammatory process; this definition excludes mechanical dilatation due to distal obstruction or due to severe acute colitis from inflammatory bowel disease, ischemic or cryptogenic colitis (toxic megacolon and reflux ileus in the setting of peritonitis).4
The incidence of Ogilvie’s syndrome is uncertain and its exact pathogenesis is also unknown, but it is due to a functional disturbance in colonic motility which is multifactorial.3,5 Most studies indicate that elderly patients are at greatest risk of developing ACPO and usually suffer preexisting medical condition. These include cardiovascular events (stroke, myocardial infarction…), metabolic abnormality (liver or renal failure, electrolyte imbalance..), drug induced (opiates, phenothiazine, antiparkinsonian agents…), infective or inflammatory events (pneumonia, acute pancreatitis…), neoplasia, postsurgical (renal transplantation, caesarean section, gynecological or pelvic surgery, same if it was released under laparoscopic,6 hip surgery), neurological disease (Parkinson, Alzheimer, multiple sclerosis…) and it can occur after a trauma: femoral fracture, spinal or pelvic trauma.1 Some other diseases can be associated to ACPO like sickle cell disease.7
The diagnosis of ACPO is based on the association of bowel obstruction and the absence of an obstacle. The clinical presentation of Ogilvie’s syndrome is not specific: abdominal distension, pain, nausea and/or vomiting, with a failure to pass flatus and stools.1 Cases which are diagnosed at the stage of colonic perforation can present sepsis symptoms and peritonitis.
To confirm the diagnosis of Ogilvie’s syndrome, many imaging explorations can be used but Abdomino-pelvic computed tomography (CT), with intravenous contrast, is the standard diagnostic test, with a sensitivity of 96% and a specificity of 93%. It confirms the presence of proximal colonic dilatation and excludes the presence of intrinsic or extrinsic mechanical obstruction.4 It also allows detecting the perforation. Barium enema can be used to diagnose mechanical obstruction but it is less frequently employed nowadays, because of the excellent yield of CT, its contraindication when perforation is suspected8 and for the possibility to resolve the obstacle due to the osmotic effect of water-soluble contrast.4
For our patient, he was treated for a Parkinson’s disease with Madopar (Madopar, ROCHE) and admitted with symptoms of bowel obstruction: nausea, vomiting and abdominal pain since a week, with distended and tympanitic abdomen. Bowel sounds were absent at the physical evaluation. The initial evaluation was based on the history and physical examination, complete blood count, serum electrolytes, renal function assessment and abdomino-pelvic computed tomography as recommended by the American Society of Colon and Rectal Surgeons.9 Abdomino-pelvic CT confirmed the colonic dilatation without any obstacle and ruled out a pneumoperitoneum, but it showed gas in the bowel wall which didn’t present any perforation. The Laboratory investigation showed elevated CRP at 167,1mg/l, without leukocytosis. These two factors associated with fever, abdominal tenderness, caecal diameter of more than 12cm for more than 6days, are all indicating factors of possible colon ischemia or perforation.4,9
In the absence of signs of peritonism, perforation or colonic necrosis that requires emergency laparotomy, the management of ACPO is not codified. Many therapeutic approaches can be considered: conservative treatment, pharmacologic treatment, colonoscopic decompression, and surgery.4 Supportive therapy must always be provided as soon as the diagnosis is made, it includes: fluid resuscitation, correction of serum electrolyte abnormalities (hypokalemia and hypomagnesemia), avoidance or minimization of all drugs delaying gut motility (such as opiates, anticholinergics and calcium-channel blockers), identification and treatment of concomitant infection, bowel rest, ambulation, knee-chest or prone positioning to promote flatus, and the insertion of nasogastric and rectal tubes to facilitate intestinal decompression.1,4,9 These measures may be continued for up to 48 to 72hours1,2,9,10 as long as the patient remains stable and has no peritoneal signs or increase in cecal diameter to 12cm.10 Success rates between 35% and 96% have been reported with these measures, and a risk of colonic perforation of less than 2.5% and a mortality ranging from 0-14%.4 Pharmacologic treatment with neostigmine is an appropriate next step for ACPO that does not resolve with supportive therapy.9 Neostigmine is a reversible acetylcholinesterase inhibitor that increases the activation of muscarinic receptors by preventing the breakdown of acetylcholine, thus improving colonic motor activity and intestinal transit; the modalities of neostigmine administration are always in debate. The respect of contraindications and cardiac monitoring is recommended during the hour following neostigmine administration.4 Endoscopic decompression of the colon should be considered in patients with ACPO in whom neostigmine therapy is contraindicated or ineffective according to the American Society of Colon and Rectal Surgeons.9 Surgery is recommended for ACPO complicated by colon ischemia or perforation or ACPO refractory to pharmacologic and endoscopic therapies.9 Patients with ACPO which have a cecal diameter >12cm for more than 6days are at risk of ischemia or colonic perforation which occur in 3 to 10% of the cases.9
For our case, the patient had ACPO for 6 days with cecal diameter at 6,79cm; supportive treatment was instituted: fasting, naso-gastric and rectal tubes, fluid resuscitation and electrolyte supply and Madopar avoiding, with favorable outcome for which neostigmine wasn’t used. Madopar treatment was resumed after resolution of symptoms and colonic dilatation on plain abdominal X-rays.
In conclusion, to the best of our Knowledge the association of ACPO and Parkinson’s disease has never been reported in literature. The diagnostic and management of Ogilvie’s syndrome in this situation follow the same recommendations concerning this pathology. The neostigmine is indicated in the absence of improvement with the conservative treatment and in case of failure, the endoscopic decompression is indicated. The surgery is restricted to the complications and after failure of previous measures.
Informed consent was taken from concerned patient
This case report was written after patient agreement
Author declares there are no conflicts of interest.
We thank all of nurses’ anaesthetists that participated on the management of this patient: Fatima Zahra Altit, Saadia Lefrais, Fatima Aithada, Younes Aouda, Rachid Cherradi, Said Elkouari.
None.

©2017 Motiaa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.