eISSN: 2373-6372


Case Report Special Issue Pancreatic Disorders
Department of Surgery, Misugikai Satoh Hospital, Japan
Correspondence: Katsura N, Department of Surgery, Misugikai Satoh Hospital, Yobuhigashimachi Hirakata, Osaka 573-1124, Japan,, Tel +81-75-983-1, Fax +81-75-971-1082
Received: May 04, 2017 | Published: September 19, 2018
Citation: Katsura N, Kawai Y. A case of sub emergent operation for salvage of severe pancreatic fistula after left hemi colectomy for advanced transverse colon cancer. Gastroenterol Hepatol Open Access. 2018;9(5):195-197. DOI: 10.15406/ghoa.2018.09.00325
Following an increase in the use of the GIATM (Covidien Co. Ltd.) stapler for treating a pancreatic stump, more preventive techniques for postoperative pancreatic juice leakage have been required. We had one successful case to salvage of severe pancreatic fistula after left hemicolectomy for advanced transverse colon cancer with pancreatic tail invasion. As the result of our proposal technique<the invagination method of pancreaticogastrostomy, grade C pancreatic fistula immediately recovered. This is simple and effective technique to prevent pancreatic fistula almost completely.
Keywords: distal pancreatectomy, pancreatic fistula, invagination method, pancreatic stump, pancreatic tumor, drain amylase
ISGPD, international study group of pancreatic fistula; CT, computed tomography; POD, post operative day
Since Billlroth first performed distal pancreatectmy in 1884,1 a lot of researchers have tried to do this operation successfully with reducing the high morbidity and mortality rates.2-4 However, unfortunately, they had been unsuccessful, and some surgeons had concluded that the operation should be abandoned.5 Furthermore, pancreatic fistula causes various complications such as abscess, hemorrhage, sepsis,6-9 and delayed gastric emptying,10 and these may result in considerable health care expenditures.11 To prevent these complications, various methods have been reported that include a standard hand-sewn suture after main pancreatic duct ligation,12 staple closure,13 sealing with glue,14 use of a seromuscular patch,15 or pancreaticoenteric anastomosis .16 However, as for now, any of them have never become a standard procedure. We have proposed new technique to prevent pancreatic fistula with invaginating pancreatic stump into stomach.17 Here, we report a case of subemergent operation for salvage of severe pancreatic fistula after left hemicolectomy for advanced transverse colon cancer invaded to pancreatic tail with our method, and lead to an excellent result.
A 69-year-old male with complaint of lower abdominal pain and extension. Colon fiber scope was performed and revealed that tumor occupied about 80% of intra-space of transverse colon (Figure 1). Enhanced CT showed large tumor from transverse colon and suspicious of the invasion to pancreatic tail (Figure 2A & 2B). At first, colostomy was done, and after patient’s condition recovered, left hemicolectomy and small cut of pancreatic tail with bipolar electric knife. As the result, we experienced the grade C pancreatic fistula (ISGPF). On day 1, drain amylase was 85,000 IU/ml. Immediately we performed our new technique showing below; after resection of distal pancreas with GIA, without any additional reinforce, to invaginate the stump to the gastric posterior wall with single layer anastomosis using 3-0 absorbable suture (Figure 3A & 3B). The anastomosis is not complicated, taking about fifteen minutes.
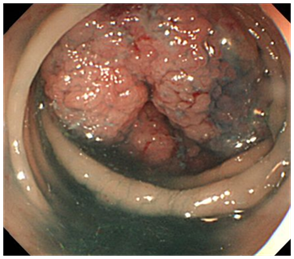
Figure 1 Colon fiber scope showed advanced tumor which almost occupied the inner space of transverse colon.
Figure 2A & 2B CT scan showed the enhanced colon tumor suspected of invasion to pancreatic tail (white circle).
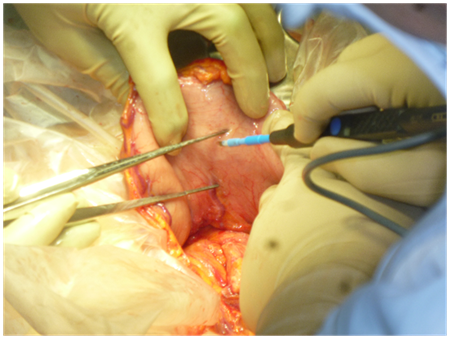
Figure 3A Cutting the posterior wall of stomach. The cutting length is 80% of the width of the pancreatic edge.
After this operation, drain amylase went down to 242 IU/ml. Drain tubes were removed on 3rd post operative day.
To prevent pancreatic fistula, various methods have been reported, including a standard hand-sewn suture after main pancreatic duct ligation,12 staple closure,13 and sealing with glue,14 use of a seromuscular patch,15 or pancreaticoenteric anastomosis.16 Sudo et al.18 reported 21cases performed the distal pancreatectomy with duct-to-mucosa pancreaticogastrostomy for preventing postoperative pancreatic fistula.18 Their method lead to no grade B and C pancreatic fistula judged with ISGPS criteria.19,20 In their report, they stated two potential factors promoting development of pancreatic fistula after distal pancreatectomy. One is extravasation of pancreatic juice from small branches of the pancreatic duct at the cut surface. The other is the increase in pancreatic ductal pressure associated with increased resistance to outflow of pancreatic juice toward the duodenum owing to contraction of the sphincter of Oddi. Variable closure techniques of the pancreatic stump, including hand-sewn, staples, sealing with fibrin glue, or covering methods, cannot completely seal the small ductal branches. The ligature of the main duct promotes a pressure gradient between the pancreatic duct and duodenum during contraction of the sphincter Oddi, which may lead to pancreatic fistula development from the ductal branches.
In this study, we performed to invaginate the pancreatic stump into the stomach by cutting the posterior wall with anastomosis by single layer. Our procedure is very simple and easy to perform within twenty minutes on the average.17 It may be natural to understand that our procedure, invaginating the pancreatic stump into stomach with single layer anastomosis, be easy and take shorter time to complete than the duct-to-mucosa pancreaticogastrostomy with an internal stenting tube and the pancreaticoenteric anastomosis.
In conclusion, the invagination method of the pancreaticogastrostomy may be a simple and effective technique for preventing pancreatic fistula development after distal pancreatectomy. Further clinical trials comparing this method with the other procedures are required to confirm its actual efficacy.
None.
Author declares that there is no conflict of interest.

©2018 Katsura, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.