eISSN: 2473-0815


Mini Review Volume 11 Issue 2
PhD in Biochemistry, Member of ISOAD, Brazil
Correspondence: Viktor I Goudochnikov, PhD in Biochemistry, Member of ISOAD, Rua Matoso Camara 73, Bairro Menino Jesus, CEP 97050-500, Santa Maria – RS, Brazil
Received: September 17, 2023 | Published: October 2, 2023
Citation: Goudochnikov VI. Shift workers in health care: endocrine age-related mechanisms of morbidity and mortality in the onto pathogenic model. Endocrinol Metab Int J. 2023;11(2):48-51 DOI: 10.15406/emij.2023.11.00331
The mini-review is presented on the role of stress mediators and melatonin in age-related morbidity and mortality, as referred to shift work in health care. A short discussion at the end of the article concerns with the ways of confronting a challenge of information overload, greatly amplified during the last years of Covid-19 pandemics. A conclusion is made on the necessity of expanding the research on stress proteins in association with processes of tiredness and fatigue, as well as in sleepiness.
Keywords: glucocorticoids, melatonin, ontogeny, shift work, stress proteins
DOHaD, developmental origins of health and disease; GC, glucocorticoids; HSP, heat shock proteins; ISOAD, International Society on Aging and Disease; SES, socio-economic status
Earlier we have discussed age-related dynamics and gender differences of morbidity and mortality in general populations of various countries.1–3 From the very beginning, we tried to understand their pathogenic mechanisms. In the present mini-review we shall consider endocrine age-related mechanisms of morbidity and mortality especially for shift workers, focusing in particular on health care.
At first we ought to remind the great relevance of this topic. In fact, modern human civilization critically depends on shift work, i.e. out of conventional regimen (approximately from 8 a.m. to 5 p.m.) and during weekends. In developed countries the fraction of shift workers is about 1/5 of the whole workforce, including policemen, security and telecommunication professionals, track drivers and aviation pilots, etc.4–6 However, in health care this fraction may be even higher, for example, approaching 1/3 in the hospitals,7 being very significant for nursing and midwifery. In addition to the lack of these professional categories in some countries like the USA,8 their “graying” (i.e. aging) in other countries, such as UK,9 becomes even more important.
Previously we have focused our attention on hormonal mechanisms of age-related diseases. In particular, we have discussed the role of glucocorticoids (GC) and other stress hormones in the mechanisms of cardiometabolic and neuropsychiatric disorders,10–12 as referred to the ontopathogenic model based on DOHaD concept.13,14 Therefore in the present article we shall pay attention especially on the importance of stress and its hormonal mediators in the mechanisms of morbidity and mortality associated with shift work.
Circadian biorhythms and their disruption in shift workers
It is well known that in humans the blood levels of cortisol are highest shortly after awakening in the morning, with subsequent decrease to nadir in late evening, close to midnight. On the other hand, the levels of melatonin in circulation are highest during nocturnal sleep, diminishing abruptly with awakening in the morning.4
In shift work, especially during night period the adjustment of circadian rhythms should occur, however this process is quite slow and rarely complete.15 As a matter of fact, the main problem of shift workers is sleepiness in the night shift and sleep disturbances during diurnal rest time. Moreover, it appears that circadian biorhythm of body temperature, with nadir at 4 a.m., almost never fully adapts to shift work. In addition, various biorhythms have different rates of adjustment in shift workers.
It means that desynchronosis, typical for shift work, adversely affects health professionals involved and represents a truly stressful situation with chronically increased levels of cortisol and decreased levels of melatonin during incorrect phases of day and night (Figure 1).16–18
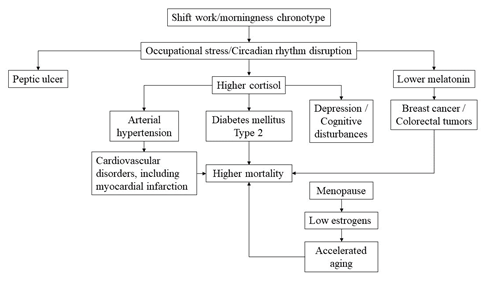
Figure 1 Pathogenic pathways involving endocrine mechanisms and probably leading, in cumulative age-related mode, from shift work to higher morbidity and mortality in health care professionals (see also explanations in the text).
The consequences of circadian rhythm disruption for morbidity and mortality
It is already well established that excessive GC levels possess both pressogenic and diabetogenic action, i.e. they increase predisposition to arterial hypertension and type 2 diabetes mellitus, the two most important components of metabolic syndrome. On the other hand, GC contribute to pathogeny of some neuropsychiatric disorders, especially to depression and dementia.10–12
Therefore, it will not be a great surprise to reveal higher tendencies of shift workers to insulin resistance and obesity, cardiovascular diseases including acute myocardial infarction and the depressive states and cognitive disturbances.4,5,19–21
In addition the disruption of circadian biorhythms in gastro-intestinal tract is quite common in shift workers, because of meal intake during the night,22 therefore such workers have the tendency to gastro-intestinal disorders including peptic ulcer and colorectal tumors.23,24 This last disorder, as well as breast cancer may be also the consequences of lower levels of melatonin, the well-known hormone with antitumor properties.25–27 As a result, in general, shift workers have higher mortality and lower longevity.5,28
If shift workers cannot easily adapt to new, frequently nocturnal regimen of work, then they tend to abuse so called social drugs like alcohol, nicotine of tobacco smoking and caffein-containing beverages (coffee, tea, soda etc.) and even some illicit drugs, such as amphetamines.5,29,30 The majority of these drugs can increase the levels of endogenous GC,31 with the consequences, at least partially, listed above.
Here it should be outlined that a small part of shift workers are better suited for nocturnal work. Especially resilient are those with so called eveningness chronotype, i.e. those who tend to sleep and awake later than average. However, with aging even this advantage can largely disappear, due to age-related tendency, in general, to morningness chronotype, i.e. with propensity to sleep and awake earlier than average.5
It appears that critical age category when shift workers begin to demonstrate higher morbidity is 40-50 years, which in women corresponds to the premenopausal period.5 Earlier we have shown that in population of the Southern region of Brazil several neuropsychiatric and gastro-intestinal disorders appear earlier than cardiometabolic ones, in middle aged (30-50 years) and advanced age groups (60-80 years) respectively.1,32
Moreover, we have shown in populations of several countries the clear indications for accelerated aging with the onset of menopause at the age of 50 years.2,33 We have suggested that these epidemiologic peculiarities may be explained, on one hand, by different age-related dynamics of some anti-stress hormones (melatonin, growth hormone) and on the other hand, by abrupt postmenopausal decrease in the levels of estrogens that possess anti-oxidant and neuroprotective properties. It means that especially women close to onset of menopause and in particular, of morningness chronotype should reconsider their capacity for shift work, for example, quitting completely or at least, moving to partial employment, as in the Netherlands.34
From all the regimens, so called rollover has essentially adverse impact on shift workers, since it challenges continuously the human ability for adaptation and adjustment.4,35 Another potentially complicating problem is low socio-economic status (SES) that per se can provoke chronic stress, due to instability of financial situation, family environment and neighborhood. On the other hand, higher morbidity and mortality in deprived, low SES persons are well known.36
Moreover, in order to survive, some health professionals try to accept shift work in at least two institutions, that together with homework may represent double and even triple ergonomic overload28 that is especially significant for pregnant women which in some countries like the USA don’t have maternity license.37 Here it is pertinent to outline that occupational stress in gestation can result in low birth weight and/or prematuriry,38 with the necessity of treatment with exogenous GC, thus programming higher predisposition to cardiometabolic disorders in the offspring.
Final comments
Although the role of stress and its hormonal mediators in programming / imprinting phenomena is rather firmly established at present,39 nevertheless it appears that hypercortisolism alone does not explain all the age-related processes. Here we must remember the mediators of cell stress including so called heat shock proteins (HSP).40,41 As a matter of fact, their contribution to the processes of tiredness and fatigue is not clear yet, nor their possible role in long-term consequences of chronic lack of sleep, as in shift workers. Nevertheless, there exist already some indications for their potential importance in aging.42 In fact, higher concentrations of GC may try to compensate for age-related decrease in HSP levels. However, the main problem here is inadequate knowledge about interactions between stress hormones like GC and stress proteins such as HSP.
In any case, shift work in health care should attract much more attention, in order to expand therapeutic potential beyond modafinil, not forgetting also that sometimes simple attitudes, such as a cup of coffee after a short nap43 can literally help in saving lives of both health professionals (especially on their way home after work shift) and of their patients, due to improvement of care quality.
With all this in mind, it is necessary to also discuss in future what kind of mental health and social services are available to help support shift workers in these conditions, as the inability to envision a life different from shift work or risking financial instability may lead to the workers feeling cornered and augmenting stress levels, risking these developing towards more concerning disorders. If addressing the root cause of much of this stress related to work and instability is not yet possible, then it is imperative to at least approach it by offering a specialized look at the psychological torment that happens in shift work, studying its effects more deeply, as well as looking into the possibility to offer mental health services as part of the benefits in shift work environments.
Notes added in proof
It is important that more recent publications including umbrella reviews44,45 largely confirm the data presented in this article. Moreover, the category of such evidence published in reviews of systematic reviews and meta-analyses has rather high significance from the points of view of both statistics and logistics, since it is based on the data gathered by many researchers in various geographic locations.
In addition, we should outline that since the year 2020, with the advent of Covid-19 pandemics the interest for studies of shift work consequences has greatly increased, because of the prolonged and frequently nocturnal involvement of many health professionals in the care of Covid-19 patients, thus amplifying their risky outcomes.46,47
At the beginning of 2021, i.e. one year after the onset of pandemics we have published a short commentary48 on interrelationship between Covid-19 and GC, the principal stress hormones, but also widely used as immunosuppressive and anti-inflammatory drugs. Just recently we tried to repeat our evaluation of this topic, but to our great surprise, in less than two years the number of articles has jumped from dozens to hundreds, in spite of quite concentrated focus of our search! Previous bibliometric analysis has already shown a great increase in the number of publications in biomedical area,49 but the novelty was much higher rate of such increase in this specific case, probably related to the critical importance of the theme of Covid-19.
Of course, open access provided by leading publishers, such as Elsevier and Wiley helped a lot (great thanks to them!), but the main problem at present is how to digest and evaluate this really huge information volume during the adequately short time?! Our proposal is perhaps to begin using softwares of artificial intelligence, not for substitution of human mental capacity, but only for essential aid to it. Therefore, the authors are ready for accepting concrete suggestions about the use of these new tools in search and analysis of published scientific data.
The author is grateful to N.V. Santos Goudochnikov for the help with Figure 1. This article was elaborated according to personal initiative without any financial support. In addition, the author affirms that conflict of interest does not exist.
Authors declare that there is no conflict of interest exists.
None.

©2023 Goudochnikov. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.