eISSN: 2473-0815


Mini Review Volume 8 Issue 6
1Endocrinology Unit, Department of Medicine, University College Hospital, Nigeria
2Dermatology Unit, Department of Medicine, University College Hospital, Nigeria
Correspondence: Taoreed Adegoke Azeez, Endocrinology Unit, Department of Medicine, University College Hospital, Nigeria, Tel 2347035728747
Received: October 02, 2020 | Published: October 30, 2020
Citation: Azeez TA, Egbu AC. Clinical profiles of thyroid dermopathy: a dermato-endocrinology minireview. Endocrinol Metab Int J. 2020;8(5):125-127. DOI: 10.15406/emij.2020.08.00294
Background: Thyroid disorders sometimes have extra-thyroidal manifestations. Hyperthyroidism is a clinical syndrome resulting from excessive secretion of thyroid hormones. The commonest cause is Graves’ disease. About 0.5 – 4.3% of patients with Graves’ disease have an infiltrative dermopathy called thyroid dermopathy. It is due to excessive deposition of glycosaminoglycans from activated fibroblasts. Skin fibroblasts are activated by thyroid stimulating hormone receptor antibodies and the whole process is initiated by T lymphocytes. Thyroid dermopathy is rarely also found in other thyroid disorders such as Hashimoto thyroiditis.
The diffuse non-pitting oedema variant is the commonest clinical presentation. Other variants include the nodular, plaque, mixed and elephantiasis types. The main concerns of the patients usually are cosmetic, discomfort and difficulty in wearing shoes. Thyroid dermopathy usually presents after the diagnosis of Graves diseases but it may present together or sometime after. Rarely, thyroid dermopathy presents before the diagnosis of Graves’ disease is made. Apart from the shin and feet, other sites that can be affected include arms, forearms, back, thighs, pinna and nose.
Conclusion: The management is multidisciplinary, involving Dermatologists and Endocrinologists. Usually, controlling the thyroid dysfunction does not translate into regression of the skin lesion. However, many patients have their thyroid dermopathy regressing spontaneously while others usually require local therapy. Other therapeutic options include systemic therapy such as pentoxifylline, compressive physiotherapy and surgery.
Keywords: thyroid dermopathy, clinical profile, dermato-endocrinology perspective
The thyroid gland is a butterfly-shaped endocrine organ located in the neck. It produces thyroid hormones which regulate metabolic activities in the body. Hyperthyroidism is a clinical syndrome caused by excessive production and secretion of the thyroid hormones. The commonly reported clinical features are heat intolerance, anxiety, excessive sweating, palpitation, fatigue, hyperdefaecation and menstrual disturbance.1 Graves’ disease, an autoimmune disorder, is the commonest cause of hyperthyroidism.2 Occasionally, it affects other organs such as the eyes and the skin. Thyroid dermopathy, sometimes called pretibial myxedema, is found in about 0.5 - 4.3% of patients with Graves’ disease.3 It is an infiltrative dermopathy diagnosed in the presence of typical symptoms and signs, biochemical evidence of thyroid dysfunction or evidence of the characteristic autoimmune markers as well as pathological findings in the skin.3 It manifests in various ways, affecting the skin of different parts of the body.
In genetically predisposed individuals, thyroid dermopathy results from an immunological cross-reaction occurring in the skin where thyroid stimulating hormone (TSH) receptor antibodies stimulate the fibroblasts in the connective tissue of the skin.4 In vitro studies have demonstrated that fibroblasts in the skin and orbit express TSH receptors on their cell surface.5
Activation of the fibroblasts make them overproduce glycosaminoglycans leading to fluid retention in the connective tissue of the skin. The antigen-antibody response is initiated by the activation of T lymphocytes. Other factors such as localized trauma and venous stasis have also been suggested to contribute to the development of thyroid dermopathy.
Histopathologically, reduced collagen fibres, extensive mucin deposition, reduced elastic tissue and oedema are the characteristic findings.3 Other rarely documented pathological features include hyperkeratosis, acanthosis and pappilomatosis.3 The pathogenesis is summarized in Figure 1 below.
Risk factors
Risk factors for the development of thyroid dermopathy are not known. However, some researchers have suggested that previous radioiodine therapy, smoking, thyroid hormonal imbalance as well as the presence of Graves’ orbitopathy could predispose an individual to developing thyroid dermopathy.6,7
Sites of thyroid dermopathy
The term ‘pretibial myxoedema’ is less favored to thyroid dermopathy because the skin lesions are found in many other areas apart from the pretibial area. The common sites documented in the literature3 and their frequency are illustrated in Table 1 below. The reasons for lower limb predilection of thyroid dermopathy are not known. Some hypotheses include gravitational forces and more fibroblasts concentration.3
|
Sites |
Frequency |
|
Pretibial Only |
94% |
|
Pretibial + Feet |
4% |
|
Pretibial + Upper Extremities |
<1% |
|
Arms |
<1% |
|
Preradial Forearms |
<1% |
|
Upper Back |
<1% |
|
Shoulder |
<1% |
|
Pinnae |
<0.5% |
|
Nose |
<0.01 |
|
Thigh |
<0.01 |
Table 1 Sites of thyroid dermopathy and their frequencies
Clinical presentation of thyroid dermopathy
Thyroid dermopathy is found mostly in Graves’ disease but it has also been documented in patients with Hashimoto thyroiditis, atrophic thyroiditis and in euthyroid individuals.6 It is also more frequently seen in females compared to males. This may be due to the fact that autoimmune thyroid disorders are generally more common in females.3 The main reasons for presentation include cosmetic, discomfort and difficulty in wearing shoes.
The temporal profile of thyroid dermopathy in relation with Graves’ disease is variable. Usually, it occurs after the diagnosis of Graves’ disease but it may predate diagnosis of Graves’ disease and they may present concurrently.3 Often, it occurs after the onset of Graves’ orbitopathy, another manifestation of Graves’ disease with similar pathophysiology. Thyroid dermopathy needs to be differentiated from lichen planus, stasis dermatitis, lichen simplex chronicus and necrobiosislipoidica. So, a review by a Dermatologist is crucial in the management of thyroid dermopathy. Figure 2 below shows a picture of thyroid dermopathy in a black patient.
Types of thyroid dermopathy
Thyroid dermopathy presents in various forms. The various clinical variants are discussed briefly below Figure 3 below illustrates the clinical variants of thyroid dermopathy and their frequencies. This is based on the findings of a retrospective study conducted by Sabanova et al.8
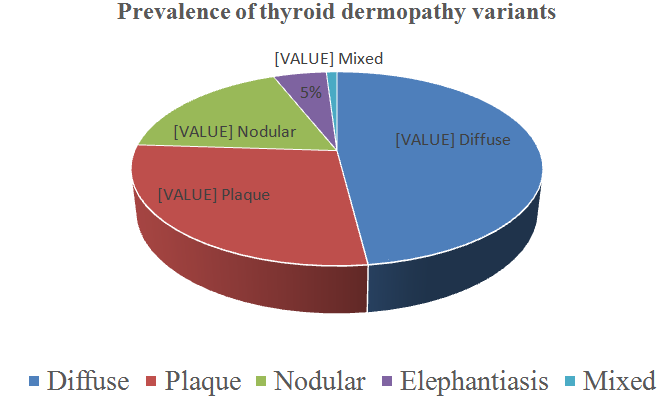
Figure 3 Thyroid dermopathy variants and their frequencies.8
Diffuse thyroid dermopathy variant usually presents as non-pitting oedema. It is the commonest variant and is characterized by induration of the skin giving the classical ‘peau d’ orange’ sign.3 In some patients, in addition to the peaud’orange sign, they also have diffuse hyperpigmented papules. Other variants are nodular and diffuse plaque types. Rarely, patients present with mixed nodular and plaque type. The elephantiasis variant, which presents like the late stage of lymphatic filariasis, has also been documented.8 This is often accompanied by significant functional disability.
Complications of thyroid dermopathy include psychological distress, superimposed bacterial infection, recurrence and entrapment neuropathy causing foot drop.3
Treatment of thyroid dermopathy
Treatment of thyroid dermopathy requires a collaborative effort from the Endocrinologist and the Dermatologist. The treatment is often challenging with many patients requiring months before regression begins but they mostly regress eventually.4 Studies have shown that control of the thyroid dysfunction may not necessarily lead to the regression of thyroid dermopathy.2 Topical steroids, and in some instances intralesional steroid, with or without occlusion, have been tried with some moderate response. In some severe variants, compressive physiotherapy as well as surgery have been adopted as therapeutic options in the management of thyroid dermopathy. Newer therapies include the use of pentoxifylline and somatostatin analogues to reduce the elaboration of glycosaminoglycans.However there is paucity of data on the outcomes of these modalities. In resistant cases, intravenous globulins have been employed. Also plasmapheresis has been tried, as documented in the literature.3
Prognosis
Largely, the prognosis is good. A study done by Schwartz et al, looking at the long term outcome of thyroid dermopathy, reported that close to half of the patients in the series regressed spontaneously, without requiring any intervention.4 Majority of the patients requiring therapy had only topical steroids or intralesional steroids and most of them significantly respond to therapy in form of partial or complete regression.
Thyroid dermopathy is an infiltrative dermopathy due to accumulation of glycosaminoglycans deposited by skin fibroblasts activated by TSH receptor stimulating antibodies. They are found in less than 5% of Graves’ disease. The commonest presentation is diffuse non-pitting oedema. Other variants include nodular, plaques, elephantiasis and the mixed types. The most common sites involved are the pretibial area and feet while other sites such as upper limbs, back and thighs are rarely involved. Thyroid dermopathy resolves spontaneously in many patients. Local therapy is the most commonly employed modality and management requires inputs from the Dermatologist and the Endocrinologist.
None.
The author declares that there are no conflicts of interest.
None.

©2020 Azeez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.