eISSN: 2473-0815


Case Series Volume 9 Issue 1
1Consultant Endocrinologist at Yuma Regional Medical Center, USA
2Hospitalist at Yuma Regional Medical Center, USA
Correspondence: Rujuta Katkar, MD, Consultant Endocrinologist at Yuma Regional Medical Center, 2851 S Avenue B, Bldg.20, Yuma, AZ-85364, USA
Received: March 25, 2021 | Published: April 2, 2021
Citation: Katkar R, Madam NR. Case series: COVID-19 infection causing new-onset diabetes mellitus? Endocrinol Metab Int J. 2021;9(1):16-18 DOI: 10.15406/emij.2021.09.00302
Objectives: This paper seeks to explore the hypothesis of the potential diabetogenic effect of SARS-COV-2 (Severe Acute respiratory syndrome coronavirus).
Case series presentation: We present a case series of observation among 8 patients of age group ranging from 34 to 74 years with a BMI range of 26.61 to 53.21 Kilogram/square meters that developed new-onset diabetes after COVID-19 infection.
Severe Acute Respiratory Syndrome Coronavirus (SARS-COV-2), commonly known as Coronavirus or COVID-19(Coronavirus infectious disease), gains entry into the cells by binding to the Angiotensin-converting enzyme-2(ACE-2) receptors located in essential metabolic tissues including the pancreas, adipose tissue, small intestine, and kidneys.
The evidence reviewed from the scientific literature describes how ACE 2 receptors play a role in the pathogenesis of diabetes and the plausible interaction of SARS-COV-2 with ACE 2 receptors in metabolic organs and tissues.
Conclusion: The 8 patients without a past medical history of diabetes admitted with COVID-19 infection developed new-onset diabetes mellitus due to plausible interaction of SARS-COV-2 with ACE 2 receptors. The resulting downregulation of ACE-2 and ACE-2 receptors expression caused islet-cell damage resulting into diabetes.
The resulting observation has the potential to adversely impact significant number of the globally affected population. Screening patients with COVID-19 for diabetes routinely can help in early detection, significantly reducing morbidity and mortality associated with diabetes.
Due to limitations of observational study with a small sample size will require further investigation in the form of Clinical trial.
Keywords: diabetes mellitus, COVID-19, ACE-2 receptors, renin-angiotensin-aldosterone system
SARS-COV-2, severe acute respiratory syndrome Coronavirus; ACE-2, angiotensin-converting enzyme-2; GAD, glutamic acid decarboxylase; RAAS, renin-angiotensin-aldosterone system.
In 2018, 34.2 million Americans, or 10.5% of the population, had diabetes.1 There is a bidirectional relationship between COVID-19 and diabetes. Not only diabetes is associated with an increased risk of severe COVID-19 but also new-onset diabetes and severe metabolic complications of preexisting diabetes, including diabetic ketoacidosis and hyperosmolarity for which exceptionally high doses of insulin are warranted, have been observed in patients with Covid-19.
SARS-COV-2, commonly known as Coronavirus or COVID-19, binds to Angiotensin converting enzyme-2(ACE-2) receptors located in essential metabolic tissues including the pancreas, adipose tissue, small intestine, and kidneys. Due to plausible alteration in glucose metabolism caused from plausible interaction of SARS-COV-2 with ACE 2 receptors downregulating ACE-2 expression, causing islet-cell damage leading to new onset of diabetes.2 New-onset diabetes was defined by initiation of antidiabetes medication or insulin among patients without diabetes at study entry.
We present a case series of eight patients admitted with COVID-19 infection and developed new-onset diabetes mellitus. They are of age group ranging from 34 to 74years, of which there where two female patients. They had a BMI range of 26.61 to 53.21Kilogram/square meters presented with symptoms suggestive of COVID-19 to our emergency department.
There was no past medical history of autoimmune diseases or other viral infections, diabetes, pre-diabetes in our patients as evidenced by lab work/HbA1c done prior to hospitalization by their primary care doctors. Two patients had past medical history of hypertension. There was no family history of diabetes in all patients.
At admission, they were diagnosed to have COVID-19 based on PCR testing. All patients had severe COVID-19 infection (defined by requiring nasal cannula oxygen therapy of more than 3litres/minute to maintain pulse saturation above 93%), which warranted their admission to the hospital. Patients were admitted anywhere between 7days to 2 weeks. Initial random blood glucose levels in the basic metabolic panel were elevated, which prompted us to check the Hemoglobin A1C, which ranged between 6.7 to 11.8%.
All patients received subcutaneous basal-bolus insulin therapy in the hospital for glucose management. As part of the COVID-19 treatment protocol in our hospital, patients received steroids, empirical antibiotics and were placed on deep vein thrombosis prophylaxis. Dexamethasone loading dose of 8 milligrams and followed by 6 milligrams daily for a total duration of 10 days was given to the patients. Once clinically improved, patients were discharged and advised to follow up with outpatient providers to monitor and manage new-onset diabetes mellitus.
All patients followed with outpatient providers, where they continued to require blood glucose-lowering treatment despite stopping getting steroids. Out of them, five patients followed up with endocrinologist had fasting C-peptide and GAD (Glutamic acid decarboxylase)-65 antibodies done, and all of them were found to have detectable C-peptide ranging between 2-3ng/ml (0.80-3.85ng/mL) with negative GAD-65 antibody levels (Table 1).
|
Age |
Gender |
Body mass index |
Smoker |
Past medical history |
Random blood glucose |
HBa1C% |
(Years) |
(kg/sq. meters) |
(mg/dL) |
|||||
1 |
34 |
Male |
34.81 |
No |
None |
490 |
11.8 |
2 |
74 |
Male |
30.67 |
Former |
Hypertension |
136 |
7.2 |
3 |
62 |
Male |
32.05 |
No |
None |
212 |
8.4 |
4 |
41 |
Male |
47 |
Former |
None |
251 |
7.5 |
5 |
40 |
Female |
53.21 |
No |
None |
189 |
8 |
6 |
62 |
Male |
26.61 |
No |
Hyperlipidemia |
115 |
6.7 |
7 |
50 |
Male |
28.34 |
No |
None |
267 |
10.4 |
8 |
53 |
Female |
36.36 |
No |
hypertension |
179 |
6.9 |
Table 1 Patient characteristics
This case series results from 8 patients' observation suggest plausible interaction of SARS-COV-2 with ACE 2 receptors and RAAS in metabolic organs and tissues play an important role in new-onset diabetes after COVID-19 infection.
ACE2 is a key counter-regulatory enzyme that degrades angiotensin II to angiotensin-(1–7), thereby attenuating its effects on vasoconstriction, increased inflammation, and fibrosis. Even though angiotensin II is the primary substrate of ACE2, that enzyme also cleaves Angiotensin I to angiotensin-(1–9), which exert opposite effects of Angiotensin II-like reduced inflamation.3
The RAAS is a hormonal system critical for maintaining blood pressure through its effect on vascular tone and aldosterone secretion. The RAAS functions at the tissue level in many organs, including the pancreas. Pancreatic cells express Angiotensin I and II receptor and prorenin genes.4 Figure 1 explains the role of amplification of ACE-2 at the pancreatic islets and the kidney.5
In human studies, tissue samples from 15 organs have shown that ACE2 is expressed broadly, including in the heart, kidneys, and the principal target cells for SARS-COV-2, the lung alveolar epithelial cells. Figure 2 explains the complex interaction between SARS-COV-2 and tissue-specific and circulating components of the Renin-Angiotensin-Aldosterone system (RAAS) that makes up a complex intersecting network of regulatory and counter-regulatory peptides.3
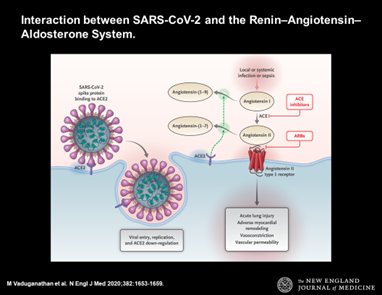
Figure 2 Explains the complex interaction between SARS-COV-2 and tissue-specific and circulating components of the Renin-Angiotensin-Aldosterone system (RAAS) that makes up a complex intersecting network of regulatory and counter-regulatory peptides.
SARS-COV-2 appears not only to gain initial entry through ACE2 receptor but also to subsequently downregulate ACE2 expression such that the enzyme is unable to exert protective effects in organs. After the SARS-COV-2 spike protein's initial engagement, there is subsequent down-regulation of ACE2 abundance on cell surfaces. Continued viral infection and replication contribute to reduced membrane ACE2 expression, at least in vitro in cultured cells.3
Activation of the RAAS within the pancreas by obesity, inflammation, or by other mechanisms like COVID-19 infection by downregulating ACE-2 expression and increasing Angiotensin II may represent a mechanism for the initiation and progression of islet-cell damage leading to new-onset diabetes mellitus.4
Observations from patients admitted for COVID-19 infection were found to develop new-onset diabetes mellitus during the hospital stay through mechanisms like SARS-COV-2 downregulating ACE-2 and ACE-2 receptors expression, causing islet-call damage resulting into diabetes.3,5
The limitations of our study are its observational study with a small sample size. Whether its type I or type II or an entirely new form of diabetes will require further investigation in the form of a Clinical trial.
Efforts in maintaining a new global registry that investigates COVID-19 and new-onset diabetes is ongoing that will help answer many questions like whether to screen patients with COVID-19 for diabetes routinely.
None.
All authors declare of no competing interests.
The study was not supported any sources of funding.

©2021 Katkar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.