eISSN: 2473-0815


Case Report Volume 1 Issue 1
1Department of Endocrinology and Diabetes Center, Metaxa, Anticancer Hospital, Greece
2Department of Pathology, Metaxa, Anticancer Hospital, Greece
Correspondence: Georgios Papadakis, Department of Endocrinology and Diabetes Center, Metaxa, Anticancer Hospital, Mpotasi 51, Pireaus 18537, Athens, Greece, Tel 00306932598392
Received: October 21, 2014 | Published: November 15, 2014
Citation: Papadakis G, Tertipi A, Papazian M, et al. Case report: primary thyroid lymphoma presenting as a rapidly enlarging thyroid mass. Endocrinol Metab Int J. 2014;1(1):4-6. DOI: 10.15406/emij.2014.01.00002
Primary thyroid lymphoma is a rarely encountered clinical entity that occurs mainly in elderly females. We present a case of B-cell origin thyroid lymphoma. The diagnosis was made by combined histology and immunochemistry. A 79-year-old woman presented with an enlarging neck mass with compression signs, dysphagia and pressure sensation around the neck. On admission, the sonogram of the thyroid gland showed an enlarged mass and CT scan demonstrated diffuse enlargement of the thyroid extending on the anterior chest wall. After total thyroidectomy, the histological investigation revealed the presence of a diffuse large B-cell non-Hodgkin’s lymphoma without other loci from the systemic staging. The patient underwent chemotherapy and radiation therapy. Clinicians should include primary thyroid lymphoma in the differential diagnosis of a rapidly enlarging thyroid mass.
Keywords: primary thyroid lymphoma, non-hodgkin lymphoma, thyroid cancer
PTL, primary thyroid lymphomas; MALT, mucosa associated lymphoid tissue
Primary thyroid lymphomas (PTL) are very rare and account for only 2.5% to 5% of all thyroid malignancies and 1-2% of all extra-nodal malignancies.1 PTL is more prevalent in females in the sixth to seventh decade of life.2 The presentation of PTL can be puzzling. PLT may be mistaken for anaplastic thyroid cancer. Immunochemistry is an important part of pathologic differentiation of these two entities.
We present here the clinical, morphological and histological features of a PTL which developed in a female patient as a rapidly enlarging thyroid mass. Finally, relevant diagnostic dilemmas are summarized.
A 79-year-old woman presented to our department reporting a recent-onset gross neck mass, throat discomfort, dysphagia, hoarseness and shortness of breath. She reported no personal or family history of thyroid disease and the symptoms had been noticed 3 months before presentation. The patient had no fever, night sweats or weight loss. The patient was nonsmoker with a remote history of cholecystectomy. The patient had no previous neck radiation exposure. The remaining medical and family history was unremarkable. Hormonal evaluation three months before the admission revealed increased thyrotropin levels [TSH 7.22μΙU/L, NR 0.3-4.5], normal thyroxine [123 μg/dl, NR 66-181] and normal triiodothyronine levels [1.81 nmol/L, NR 1.1-3.1]. The antithyroglobulin antibodies were increased (anti-Tg 109 IU/ml, NR<60) and antithyroid peroxidase antibodies were normal (anti-TPO 45 IU/ml, NR<60). The initial sonogram indicated multinodular goiter and a gross heterogeneous hypoechogenic mass on the left lobe (maximum diameter 38mm) compatible with lymphocytic thyroiditis. FNAB was not suggested and the patient was prescribed L-thyroxine 50μg replacement therapy daily.
On admission three months later, the symptoms deteriorated. Clinical examination revealed a firm, immobile and painless mass descending in the anterior chest wall. The laryngoscopy revealed left vocal cord palsy. Biochemical investigation was normal. A new sonogram was performed which revealed a 21 x 26 mm solid mass on the right lobe and a 26 x 29 mm solid mass on the left lobe. The masses were strongly hypoechoic, heterogeneous intermingled with echogenic structures. These features are related to thyroid lymphoma.3 Enlarged neck nodes were observed on both sides. The patient underwent a fine needle aspiration biopsy with a 23G needle and the cytologic analysis showed thyrocytes, lymphoid elements and atypical nuclei. The histopathologic evaluation for CD-45 was negative (nearly all large B-cell lymphomas are CD-45 positive).
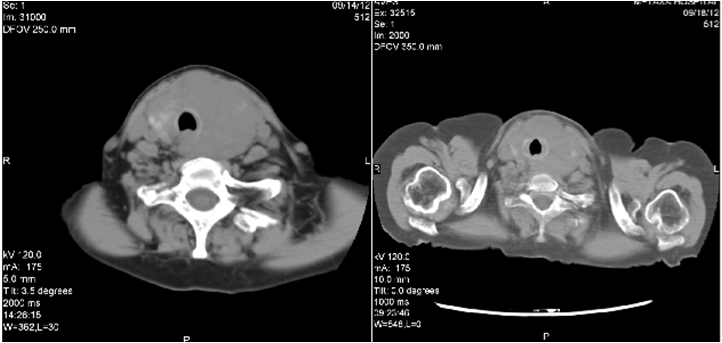
The patient underwent imaging of the neck for further evaluation. CT demonstrated marked enlargement of the thyroid gland, left greater than right. There was mass effect on the trachea, decreased diameter of the trachea and enlarged neck nodes (Figure 1). The patient underwent total thyroidectomy.
Combined histological and immune histological analyses led to the diagnosis of la diffuse large B-cell lymphoma of the follicular centre/ activated like-cell-non GCC, with a high proliferation index (Mib1/Ki-67 : 90%) , positive LCA(CD45Rb), CD10, CD75, CD79a, BSAP, BCL6, BCL2, MUM1, k-light chain, p53 and p63 and negative reaction of the neoplastic cells for CKAE1-3, EMA, HBME1,Thyreogloboulin, Galectin-3 and others (Figure 2).4
Evaluation for systemic disease with thorax, abdomen and pelvis imaging and bone marrow aspiration excluded other neoplastic foci. According to the Ann Arbor guidelines for primary thyroid lymphoma the patient had stage IIE disease at diagnosis (involvement of the thyroid and lymph nodes on the same side of the diaphragm). After surgery the patient underwent systemic chemotherapy with the R-CNOP chemotherapeutic protocol, i.e. rituximab (anti CD-20 antibody) 580mg, mitoxandrone 15 mg, cyclophosphamide 1160 mg, vincristine 2mg and methylprednisolone 16mg cumulative dose. Radiation therapy was planned after the chemotherapy cycles. The post-chemotherapy CT scan showed a marked regression of the mass with decompression of the trachea (Figure 3).
We describe an unusual case of a PTL. Within the population, this disease is estimated to occur at an annual incidence rate of 2.1 persons per million. PTL is associated with a poor prognosis.5 Most thyroid lymphomas are of B-cell origin. Mucosa associated lymphoid tissue (MALT) is recognized as a distinct lymphoma with unique clinopathological features and follicular lymphoma is another very rare subtype.
Chronic lymphocytic thyroiditis or Hashimoto’s disease is found in more than 90% of the reported cases.6 Some authors hypothesize that chronic stimulation of lymphocytes by thyroiditis leads to malignant transformation. In our patient antithyroglobulin antibodies were increased in multiple blood tests. Most patients with PTL are euthyroid at initial presentation and 10% present with hypothyroidism.7
On presentation, the clinical findings of our patient orientated us to consider anaplastic carcinoma of the thyroid. Most patients with PTL have a rapidly growing painless thyroid mass causing compressive symptoms. These symptoms overlap with that of the anaplastic thyroid carcinoma.8 The unexpected histological examination changed the initial diagnosis. The diagnosis of a primary thyroid B-cell lymphoma was established after exclusion of systemic involvement.
FNA is an essential tool in the diagnostic workup of thyroid disease,9 although FNA yields inconsistent results in the diagnosis of thyroid lymphomas and its diagnostic accuracy varies widely. This is due to the histopathological similarities between primary thyroid lymphoma and Hashimoto’s thyroiditis.10 The gold standard for histologic diagnosis is considered the core needle biopsy or surgical biopsy. In our patient the FNAB was non-diagnostic and the cell immunohistochemistry for CD-45 was not positive to establish the diagnosis. FNAB should not replace open thyroid biopsy which is important for the confirmation and sub typing of the disease. Currently, a larger percentage of patients undergo surgery in order to achieve precise histological diagnosis.11 In our patient thyroidectomy was useful for the management of compressive symptoms and for the histological diagnosis.
Chemotherapy followed by radiotherapy is considered the standard treatment.12 Surgery that was once the mainstay of treatment for PTL plays now a minimal role. Total thyroidectomy exposes unnecessarily the patient to the risks of surgery, such as recurrent laryngeal nerve damage and hyperparathyroidism without conferring any survival advantage. Thyroidectomy is useful for the management of compressive symptoms of the trachea and the esophagus and severe airway obstruction. Logo regional treatment with surgery is the primary treatment of localized MALT lymphomas.
In conclusion, we describe a very rare case of primary thyroid lymphoma. Our report emphasizes the need for clinical awareness in such perplexing cases which clearly require a multidisciplinary approach.
None.
The authors have nothing to disclose, and there is no financial interest or any conflict of interest.

©2014 Papadakis, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.