eISSN: 2473-0815


Research Article Volume 11 Issue 1
UDELAR/Hospital de Clínicas, Montevideo Uruguay
Correspondence: Fabrizzio Girardi, UDELAR/Hospital de Clínicas, Montevideo, Uruguay
Received: May 16, 2023 | Published: July 5, 2023
Citation: Girardi F, Parada U, Guarneri C. Brown tumor secondary to primary hyperparathyroidism. Clinical case, set-up and role of the surgeon. Endocrinol Metab Int J. 2023;11(1):18-21 DOI: 10.15406/emij.2023.11.00326
This work is focused on describing the most important characteristics of primary hyperparathyroidism and the bone involvement that this pathology produces, based on a clinical case of a patient attended at the Hospital de Clínicas (UDELAR) - Montevideo-Uruguay.
Brown tumors (PT) are a rare abnormality of bone tissue caused by chronic hypersecretion of parathyroid hormone (PTH), the pathophysiology of which will be discussed throughout the text.
They manifest clinically as tumors, which is of paramount importance since it is necessary to evaluate differential diagnoses. It frequently develops in long bones, which explains its topographic variability.
The treatment of these lesions depends fundamentally on the control of hyperparathyroidism and the location of the tumor. Most of them remit when PTH levels are normalized.
Keywords: hyperparathyroidism, tumor pathologies
Primary hyperparathyroidism (PHP) is an endocrine pathology characterized by the loss of regulation of extracellular calcium concentration, in which one or more parathyroid glands produce and secrete excessive parathyroid hormone causing a state of sustained hypercalcemia. The most frequent cause is due to a single adenoma (85% of cases) and multiple adenomas in a smaller proportion.1
The diagnosis of PPH is biochemical, characterized by humoral PTH and calcemia dosage. The context of chronic hypercalcemia favors the development of bone involvement, and brown tumors may develop.
The first report of brown tumors also called osteitis fibrosa cystica was made in 1891, it is a very rare bone alteration, generally localized and destructive in the bone sector where it settles, of slow growth, non-neoplastic, secondary to an over production of PTH chronically maintained. This condition makes the osteoclastic state predominate over the osteoblastic one, causing bone resorption and filling of the degraded area with connective tissue and hemosiderin, expressing itself clinically as a painful tumor on a bone structure and in the most severe cases is associated with pathological fracture.2
The treatment of choice when primary hyperparathyroidism is associated with brown tumor is parathyroidectomy (single adenoma) or pathological glands (multiple adenoma). The resection of the pathological parathyroid in the great majority of cases causes the osteitis fibrosa cystica to disappear.3
In cases in which the patient's field does not allow an anesthetic-surgical procedure or if the patient refuses to undergo surgery, there is alternative medical treatment. These are based on systemic and/or intralesional corticoids at the level of the brown tumor, as well as the use of calcitonin, emphasizing that these non-surgical treatments have a lower success rate in relation to parathyroidectomy.4,5
This work focuses on bone involvement (brown tumors) produced by chronic hypercalcemia secondary to hyperparathyroidism.
We describe the clinical case of a 43-year-old male patient, whose personal history was smoking and epilepsy, who was being followed by a neurologist. His reason for consultation was the appearance of a lump on his right leg.
As for the functional aspect, he highlighted as elements of current disease the appearance of a tumor of 1 year of evolution with slow and progressive growth, painless, accompanied by diffuse bone pain, without episodes of pathological fractures. No lumbar pain or history of nephritic colic.
Physical examination: performance status of 0, long-limbed, hemodynamically normal, without tumors in the cervical region. In the right lower limb, there was a tumor in the middle third of the leg, with clear limits, oval, painless, hard, about 5 cm in diameter, major axis, immobile, with no signs of flux in the covering planes (Figure 1).
The PTH dosage was 914ng/dL (reference value <60ng/dL). Ionogram altered at the expense of hypercalcemia (12.3mg/dL).
Preoperative localization imaging studies were performed:
Cervical ultrasound: hypoechogenic nodule of 4cm, in posterior region at the level of the lower third of the left thyroid lobe. Thyroid gland without alterations.
Parathyroid scintigraphy with Technetium 99 sestamibi and SPECT: Hypercaptured left lower parathyroid tissue (Figure 2).
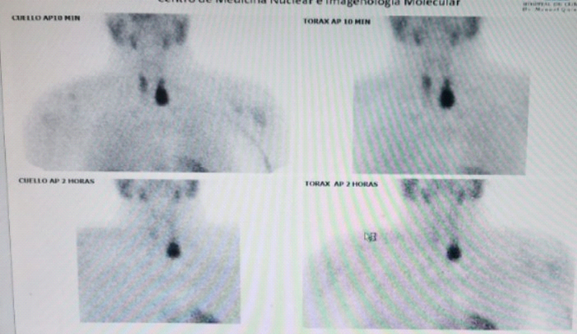
Figure 2 Persistence of radiolabel at the level of the left inferior parathyroid gland is observed with the passing of time of evaluation.
Valuation is completed: X-ray of the right leg: it highlighted the presence of a radiolucent lesion, with well-defined, clear borders, associated with discrete thinning of the adjacent bone cortex (subperiosteal resorption) and poor reactive bone tissue around it (Figure 3).
A biopsy of a tumor in the right lower limb was performed in order to confirm the presumptive clinical diagnosis and rule out other differential tumor pathologies. The anatomopathological result was compatible with brown tumor, so a diagnosis of osteitis fibrosa cystica was made.
The patient's clinical case was discussed in a multidisciplinary meeting with the participation of different departments (internal medicine, nephrology, imaging, general surgery, pathological anatomy, nuclear medicine), and it was decided on that occasion to perform surgical treatment by means of left lower parathyroidectomy.
A mini-incision approach was performed guided by ultrasound identification of the pathologic parathyroid gland prior to surgery (Figure 4) (Figure 5).

Figure 4 & Figure 5 Parathyroid adenoma evidenced in cervical ultrasound performed in the surgical block room. Right image: the site where the parathyroid adenoma should be topoographed in the deepest cervical planes was marked with a skin demographic.
A PTH sample was taken prior to the start of surgery and another one 15min after the pathological gland was resected, showing a decrease (914 ng → 178ng).
She is currently under clinical-humoral-imaging control, with a clear decrease of the brown tumor. Calcemia and PTH dosage are in the normal range (Figure 6).
The increased secretion of PTH from the parathyroid glands is called PPH. In PPH the alteration is in the parathyroid gland itself.
Primary hyperparathyroidism is one of the most frequent endocrinological diseases, predominantly in patients over 50 years old, and in famales. Its etiology in order of frequency is due to parathyroid adenoma (as in the case of our patient), parathyroid hyperplasia, multiple adenomas and parathyroid carcinoma.6
The diagnosis of (PPH) is by means of biochemical laboratory studies in which an increase in the serum concentration of parathyroid hormone (>60ng/dL) and hypercalcemia (>10.2mg/dL with azoemia and creatininemia) are observed.6 We emphasize that hypercalcemia levels above 14 mg / dL increase the risk of developing calciphylaxis (cutaneous ischemia secondary to obstruction by calcification of the skin microvasculature).7
The state of chronic hypercalcemia without treatment or without response to medical treatment favors the development of alterations in different parenchyma: (bone demineralization - osteoporosis), renal (renal lithiasis, acute or chronic renal failure, cardiovascular (conduction disorders, myocardial calcification, heart failure), gastrointestinal (visceral hypo-motility - constipation), and neurological (neuropsychological disorders).
Brown tumors are a very rare bone manifestation of chronic hyperparathyroidism, generally paucisymptomatic. The diagnosis is clinical, imaging and anatomopathologic confirmation.
The bone lesions we are analyzing can be single or multiple, they tend to settle more frequently in long bones, and can cause complications such as pathological fractures at the level of the affected bone. When they are topographically located in the head and neck region, especially in the facial mass, they are most frequently located at the maxillary level.8,9
The pathophysiological process of brown tumors is proposed as a chronic state of (HPP), which causes a situation of maintained PTH hypersecretion. The activation and maturation of osteoblasts into osteoclasts
Causing bone resorption, with a consequent increase in serum calcium. As a consequence, microfractures are produced, small hemorrhages in the area that determines the deposit of connective tissue and hemosiderin. Its clinical translation is the appearance of a tumor whose bone topography is variable.10
A correct diagnostic evaluation is of utmost importance when faced with this type of tumors, since it is essential to rule out differential diagnoses of malignant neoplasms such as chondrosarcomas, osteosarcomas, entities with worse prognosis, but other differential diagnoses of benign bone neoplasms such as giant cell bone tumors, solid aneurysmal bone cyst and giant cell reparative granuloma must also be ruled out.11
Humoral results support the diagnosis of brown tumors, when there is elevated alkaline phosphatase concentration, increased PTH associated with hypercalcemia, hypophosphatemia and decreased Vitamin D dosages.
The surgical success rate has improved due to better preoperative localization of the pathologic glands. Concomitantly, the cervical mini-incision approach (1.5-2cm) centered on the pathologic parathyroid gland improved the esthetic result, reduced the operative morbidity and mortality, the operative time and the hospital stay.
The advantages of this mini-incision are based on minimal dissection down to the parathyroid gland by directed access, allowing indemnity of the recurrent laryngeal nerve and the parathyroids on the side contralateral to the approach.
Regarding preoperative localization studies we highlight
Cervical ultrasound: non-invasive, technically dependent, accessible study, whose diagnostic sensitivity for parathyroid pathology is between 70-88%. It allows to obtain macroscopic data of the pathological parathyroid glands, its topography, relation to the thyroid lobe, and to investigate and/or discard alterations of the thyroid gland. We emphasize that parathyroid glands of normal size are very difficult to recognize by ultrasound because of their small size. It is important to have an expert technician in cervical ultrasound since it improves the recognition of pathological glands.12
Gammagraphy associated with 99mTc-sestamibi tomography (SPECT-CT): an objective, radiant, functional and anatomical study, which has greater diagnostic precision for topography of the pathological parathyroid gland and is very useful for ectopic localizations.13
Positron emission tomography scintigraphy with 11C-methionine: it is a study with greater topographic sensitivity, used to detect parathyroid adenoma when it could not be located by other imaging methods.14
Cervical 4-dimensional computed tomography is a second-line technique for the identification of parathyroid adenomas, when ultrasound and SPECTC fail to objectify.
Advances in medical technology and greater diagnostic sensitivity of the aforementioned imaging tools have boosted the trend of the mini-incision surgical approach. The preoperative diagnostic accuracy allows a directed approach and dispenses with bilateral cervical exploration in a systematic way, decreasing the risk of neck hematoma, nerve injury and glandular revascularization.15
The PTH dosage prior to surgery and 15 minutes after resection of the gland allows the surgeon to audit the procedure, the objective being a decrease of at least 50% of the initial PTH level.16
Complementarily, immunofluorescence by administration of intravenous indocyanine green allows visualization of the pathological parathyroid gland using an infrared device.
Other intraoperative identification methods can also be used, such as radio guided resection by radiotracer or auto fluorescence device.17
The treatment of parathyroid tumor is based on the control of hypercalcemia secondary to hyperparathyroidism. Resection of the pathological parathyroid gland restores both parathyroid hormone and calcium to normal values. This fact generates the deactivation of the osteoclastic activity, achieving in most cases the remission of the brown tumor in the postoperative.
PTs are rare pseudo-tumors of the bone. The treatment of these lesions depends fundamentally on the control of hyperparathyroidism and the location of the tumor. Most of them remit when PTH levels are normalized.
The surgeon with experience in endocrine surgery plays a fundamental role in intraoperative identification, managing to resect the pathological GP with a minimal incision and dissection, avoiding injuries to noble structures.
None.
Authors declare that there is no conflict of interest exists.
None.

©2023 Girardi. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.