eISSN: 2473-0815


Case Report Volume 11 Issue 3
1Physical Medicine and Rehabilitation Physician, Medicine and Rehabilitation Center - Rovisco Pais, Portugal
2Internal Medicine Physician, Local Health Unit of Matosinhos - Pedro Hispano Hospital, Portugal
Correspondence: Carolina Paiva, Physiatry Resident, Physical Medicine Centre - Rovisco Pais, Portugal
Received: October 17, 2023 | Published: October 25, 2023
Citation: Paiva C, Assunção S, Moreira S, et al. Beyond bipolar disease: primary hyperparathyroidism in a bipolar patient. Endocrinol Metab Int J. 2023;11(3):53-55 DOI: 10.15406/emij.2023.11.00332
Primary hyperparathyroidism consists of a dysregulated production of parathyroid hormone that results in abnormal calcium homeostasis. It is mostly detected in the asymptomatic phase; however, presentation may include a broad spectrum of clinical manifestations. We describe the case of a 67-year-old female patient with a previous history of bipolar disorder and several vascular risk factors who presented with generalized muscular weakness, anorexia and weight loss, polydipsia, nausea, constipation and mental confusion with behavioural change. Mental and behaviour changes were previously considered a cognitive deficit. Blood tests revealed severe acute renal injury, severe hypercalcemia and frankly increased parathyroid hormone. During hypercalcaemia study, cervical ultrasound identified a nodule compatible with parathyroid adenoma, coincident with hypercaptant focus on the sestamibi scintigraphy. Patient underwent treatment with zolendronic acid and posterior parathyroidectomy with gradual symptomatic and analytical improvement. The authors report this case recalling that psychiatric pathologies can delay the diagnosis of physical conditions.
Keywords: hyperparathyroidism, parathyroid hormone, hypercalcemia, adenoma, bipolar disorder, parathyroidectomy
Primary hyperparathyroidism is a common endocrine disease, more common in females and in the fifth decade of life, which is characterized by an autonomous secretion of parathyroid hormone (PTH) from one or more parathyroid glands. Such dysregulation typically leads to hypercalcemia and too high or inappropriately normal PTH concentrations for the calcium value.1–3
The majority of cases of primary hyperparathyroidism, excessive PTH production is caused by a single parathyroid adenoma. Much less frequently, it is due to multiglandular hyperplasia or parathyroid carcinoma.1,4
The clinical presentation has evolved over the last 40 years, as biochemical screenings have become a routine practice, and currently it is mainly diagnosed in the asymptomatic phase. In developed countries, with structured health systems focused on disease prevention and screening, it is uncommon the clinical presentation with obvious symptoms.2,3 However, on rare occasion, presentation may include a wide spectrum of calcium homeostasis disorders, from parathyroid crisis (severe and markedly symptomatic hypercalcemia) to normocalcemic hyperparathyroidism.5,6
Symptoms and signs, when present, reflect the combined effects of excessive PTH secretion and hypercalcemia. Neuropsychiatric and neurocognitive symptoms are frequently encountered however, the pathophysiological basis of these changes and their relationship with the disease are not yet fully understood.2,7
Authors present the case of a 67-year-old Caucasian woman with previous history of bipolar disease who was referred to the emergency department (ED) after being found fallen, unable to get up due to muscle weakness. She reported asthenia, polydipsia, nausea and anorexia with weight loss, and constipation that had lasted two months. Family also reported greater mood fluctuations, disorientation, amnesia and changes in behaviour since that time. Due to these behaviour changes, she had been reevaluated in Psychiatry consultation and the possibility of dementia syndrome onset was considered.
Upon admission do the ED, patient was conscious and cooperative, disoriented in space and time, with confused and confabulatory speech. Pale and dehydrated skin and mucous membranes was observed, and patient also presented generalized muscle weakness that limited functional capacity, although no strength asymmetries or preferential functional loss of the shoulder or pelvic girdles were present. Laboratory studies found metabolic acidaemia with pH 7.26 and hyperlacticaemia of 5.10 mmol/L, significant elevation of myoglobin (2332.4ng/mL), hypercalcemia with ionized calcium of 2.09 mmol/L (N 1.15-1.35mmol/L) and grade 3 acute kidney injury (AKIN) with creatinine of 3.2mg/dL (Table 1).
|
Blood gas FiO2 21% |
Biochemistry |
Blood count |
|
pH 7.26 |
Urea 169 mg/dL |
Hemoglobin 12,7 g/dL |
|
pO2 93mmHg |
Creatinine 3.2 mg/dL |
MCV 94,4 fL |
|
pCO2 34 mmHg |
Sodium 139 mEq/L |
MCHC 32,5 g/dL |
|
Bicarbonate 16,5 mmol/L |
Potassium 5.0 mEq/L |
Leukocytes 12,25/Ul |
|
Oxigen Saturation 96% |
AST 28 U/L |
Neutrophils 77,90% |
|
Calcium 2.09 mmol/L |
ALT 12 U/L |
Platelets 156000/uL |
|
Lactate 5.10 mmol/L |
RCP 5.30 mg/L |
- |
|
Blood sugar 253 mg/dL |
Troponin I 114.30 mg/dL |
- |
|
- |
Mioglobin 2332,4ng/mL |
- |
Table 1 Laboratory study upon admission to the emergency department
The clinical condition was initially assumed as an acute confusional state due to psychiatric decompensation, and the acute kidney injury with metabolic acidaemia was interpreted in the context of hypovolemia and rhabdomyolysis. Patient was hospitalized under fluid therapy. Transient improvement in renal function and resolution of rhabdomyolysis and metabolic acidosis was observed. However, the remaining symptoms persisted, and patient also developed nausea and vomiting, persistent constipation despite several laxatives, hypernatremia, polyuria and polydipsia compatible with nephrogenic diabetes insipidus. Laboratory studies revealed an aggravation of hypercalcemia with ionized calcium 2.52mmol/dL, mild hypomagnesemia and hypophosphatemia, vitamin D deficiency and a very high parathyroid hormone (PTH) value of 951.69g/mL (N 15-68.3g/mL) (Table 2).
|
Calcium 2.52mmol/dL |
|
Magnesium 1.22 mg/dL (N 1.6-2.6mg/dL) |
|
Phosfate 1.4mg/dL (N 2.3-4.7mg/dL) |
|
Vitamin D 6 ng/dL (low) |
|
Parathormone 951.69g/mL (N 15-68.3g/mL) |
Table 2 Laboratory study at day one of hospitalization
From the study of hypercalcemia with hyperparathyroidism, a cervical ultrasound was performed which confirmed the presence of a nodule suggestive of left parathyroid adenoma (Figure 1) coinciding with the focus of uptake on sestamibi scintigraphy (Figure 2). Primary hyperparathyroidism with hypercalcemia was identified, which could justify the overall clinical picture. The recent worsening of behavioural changes and mental confusion were also interpreted in the same context. A month later, patient underwent left lower parathyroidectomy (Figure 3), and histology revealed parathyroid adenoma (Figure 4).
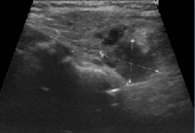
Figure 1 Cervical ultrasound showing a hypoechogenic nodular structure (20x9mm) posterior to the left lobe of the thyroid, compatible with parathyroid adenoma.
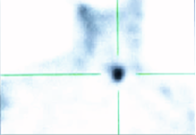
Figure 2 Parathyroid scintigraphy revealing an anomalous radiopharmaceutical uptake in the projection of the left lobe of the thyroid (posterior to it, in SPECT tomographic images), compatible with hyperfunctioning parathyroid tissue, possibly adenoma of the left parathyroid gland.
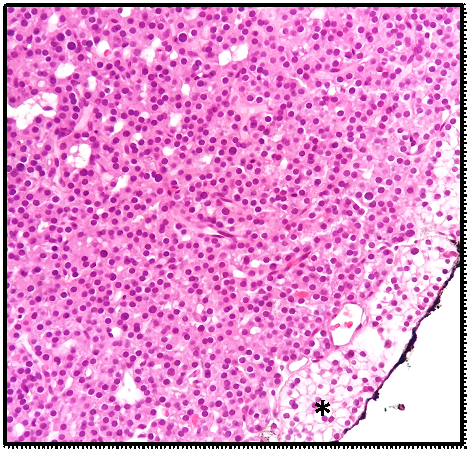
Figure 4 Main cells arranged in towel and in microfollicles compressing normal parathyroid tissue to the periphery (asterisk) with Chinese ink on the external surface.
At the time of discharge calcium and PTH levels had been corrected and the patient had regularized gastrointestinal transit and urine output, good food tolerance, recovery of muscle strength, and more coherent and oriented speech with functional improvement compared to the pre-admission period, despite maintaining labile mood characteristic of bipolar disorder.
The prevalence of classic hyperparathyroidism changes caused primarily by increased PTH, namely nephrolithiasis and bone disease, has been decreasing.1–3 Hypercalcemia itself can cause a wide spectrum of renal, gastrointestinal, musculoskeletal, neurological and cardiovascular manifestations, including nephrogenic insipidus diabetes, anorexia, nausea and vomiting, constipation, muscle weakness and fatigue.8,9
The association of hyperparathyroidism with neurocognitive and neuropsychiatric symptoms has been studied. Symptoms such as anxiety, depression, memory changes, concentration deficit and cognitive decline are frequently observed in patients with primary hyperparathyroidism, and more serious neuropsychiatric conditions such as confusional syndromes and psychotic conditions may develop.2,4 The pathogenesis of this symptoms remains unclear; however, calcium is thought to play a central role in determining changes in monoamine metabolism in the Central Nervous System, thereby modifying neurotransmission and resulting in alterations in mood and cognition.10
Primary hyperparathyroidism diagnosis is likely in the presence of a high calcium level along with elevated or inappropriately normal PTH level.1 Imaging methods are not diagnostic, and their use is recommended only when surgical treatment is planned, helping to identify abnormal parathyroid tissue.1,2 The most commonly used techniques are ultrasound, computed tomography and scintigraphy.1
Parathyroidectomy is the only curative treatment, allowing normalization of calcaemic and PTH values, with consequent resolution of related symptoms. It also promotes stabilization/regression of bone and renal complications.11–13 Some studies have also showed improvement/resolution in neurocognitive and neuropsychiatric symptoms after parathyroidectomy.14,15
The timing of symptom improvement after parathyroidectomy has not been well characterized. While certain symptoms exhibit improvement or resolution as early as 1 week postoperatively, others may take 6 weeks, and it is uncommon for symptoms to show significant improvement or resolution beyond this time.16
This case illustrates an uncommon presentation of primary hyperparathyroidism with severe hypercalcemia that by itself caused a wide spectrum of symptoms. It is understood that the fact that the patient had history of bipolar disease somehow delayed the diagnosis since memory and behavioural changes were initially interpreted in context of psychiatric illness. On the other hand, upon admission, the patient presented with metabolic acidaemia with several contributions, and hypercalcemia was not immediately taken into account. Despite the importance of stabilizing the patient before planning the entire diagnostic approach, this case reminds the importance of recognizing and treating calcium disorders in time.
This case demonstrates the importance of clinical reasoning. It was an outside the box reasoning that allowed to encompass symptoms attributable to a single cause and to admit that sometimes acute neuropsychiatric changes in psychiatric patients have an organic cause.
None.
Authors declare that there is no conflict of interest exists.
None.

©2023 Paiva, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.