eISSN: 2473-0815


Case Report Volume 2 Issue 1
Department of Pediatric Endocrinology, Central Teaching Hospital for Pediatrics, Iraq
Correspondence: Ali HasanDhari Al Jumaili, Department of Pediatric Endocrinology and Diabetes center, Central Teaching Hospital for Pediatrics, Baghdad, Iraq
Received: March 20, 2015 | Published: April 20, 2015
Citation: Jumaili AHDA. A rare case of virilizing adrenocorical carcinoma in a child presented with peripheral precocious puberty. Endocrinol Metab Int J. 2015;2(1):49-51. DOI: 10.15406/emij.2015.02.00010
Objective: To report a rare case of virilizing adrenocortical carcinoma presenting with peripheral precocious puberty.
Methods: we present the initial clinical findings, laboratory tests and medical imaging findings with surgical procedure, tumor staging and histopathological study. Post-operative follows up schedule and management. In addition a brief review literature
Results: A 8.5 year old boy presented with pubarche and other virilizing features that dated back to one year. Physical examination revealed; height 121 cm, weight 30 kg, Tanner Stages for pubic hair, penile length and testes volume were IV, IV, ІI respectively. Laboratory findings gonadotropins were low, testosterone high so the precocious puberty was gonadotropins independent (peripheral) either adrenal or testicular, so abdominal ultrasonography performed that showed well defined mass at right suprarenal region (49×48) mm., and abdominal magnetic resonance demonstrated a mass at right adrenal gland region measures (5×5) cm then dynamic computed tomography of adrenal glands revealed: right adrenal mass (5×4x4) cm well defined. Scrotal ultrasonography revealed both testes slightly enlarged in size with normal echogenicity. Based on the above data the interpretation was adrenal androgen-secreting tumor either adenoma or carcinoma. Therefore, the patient underwent right open adrenalectomy: grossly; encapsulated mass, no invasion to surroundings, size (5×4x4). Histopathology study was consistent with adrenocortical carcinoma confirmed by Immunohistochemistry. Postoperatively: glucocorticoid replacement therapy was initiated, and he was scheduled for follow –up examination.
Conclusion: This case illustrates the rare occurrence of adrenocortical carcinoma in this age group and to our knowledge is the first case report in Iraq.
Keywords: Peripheral precocious puberty, Adrenocortical carcinoma, Gonadotropins
Adrenocortical carcinomas are rare tumors that have a bimodal distribution; the first peak is in children less than five years and the second around the fifth decade.1 Although most adult adrenocortical carcinomas are non-functional, in the pediatric age group, nearly 95% are functional virilization is the most common abnormality and Cushing’s syndrome and hyperaldosteronism are less frequent. Incidence, annually (0.1-0.4 cases/million/year) and malignant adrenal tumors comprise approximately 1% of all carcinomas diagnosed prior to 20 years Data have suggested an increased incidence in female individuals, especially at age 0-3 years or after age 13 years.2
A 8.5- year-old boy presented with excessive pubic hair and other features of virilization for one year duration. On examination: he looks well, normal blood pressure, the height 121 cm (above 50th percentile), weight 30kg (75th percentile). Tanner stages for pubic hair, penile length (10cm) and testes volume (3 ml) were IV, IV, ІI respectively. No palpable abdominal mass, the rest of his physical examination unremarkable. Laboratory findings: FSH˂ 0.10 IU/L (1.4-15.4), LH 0.15 IU/L (1.2-7.8), testosterone 8 nmol/l (0.10- 1.04), 17 hydroxyprogesterone 2.1 ng/ml (0.2-3.5), cortical 346 mMol/L (168-728) ,Thyroid function tests, renal function tests and serum electrolytes were all normal. Imaging data: Bone age 11 years, abdominal ultrasonography showed well defined mass at right suprarenal region (49×48) mm., abdominal magnetic resonance demonstrated a mass at right suprarenal region measures (5×5)cm (Figure 1A) & (Figure 1B). Dynamic computed tomography of adrenal glands revealed: right adrenal mass (5×4x4)cm well defined associated with perilesional vessels, no invasion to surrounding structures. Brain magnetic resonance imaging was normal. Scrotal ultrasonography revealed both testes slightly enlarged in size with normal echogenesity chest X-ray normal. Based on the above data the interpretation was adrenal androgen-secreting tumor either adenoma or carcinoma. Therefore, the patient underwent right open adrenaloectomy: grossly; encapsulated mass, no invasion to surroundings, size (5×4x4). Histopathologic study was consistent with adrenocortical carcinoma confirmed by Immunohistochemistry (Figure 2 panel A) & (Figure 2 panel B). Postoperatively , on the first day, the patient complained of fatigue, and was found to have an undetectable morning serum cortisol level of ˂0.500 nmol/L (N: 171-536), Thus glucocorticoid replacement therapy was initiated, and he was scheduled for follow–up examination monthly for the first two years , scanning every 3 months for the first two years, 4 months for the next 2 years and every 6 months during the fifth year, since surgical treatment the patient has reported decreasing in features of virilization
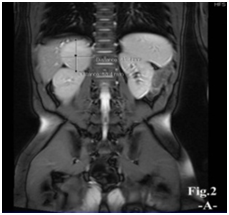

Figure 1 Magnetic resonance images, revealing well-defined mass at right suprarenal region, measures about (5×5)cm.
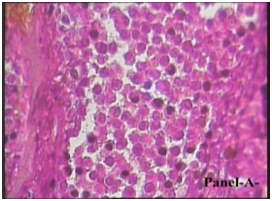

Figure 2 Adrenal mass biopsy section stained with hematoxylinand eosin( panel A) shows malignant tumor composed of solid sheets of atypical cells with dense compact eosinophillic cytoplasm, some cells have haveintranuclear inclusion, more than five mitosis per 50/HPF, capsular invasion, sinusodial invasion, focal clear cell component and broad fibrous bands.
Adrenocortical carcinoma is a rare tumor in the pediatric population (0-21 y)1 in most cases, the patient’s history includes elements of adrenocortical hormone production and a palpable mass2,3 in our case presented with features of virilization alone. A similar case report of adrenocortical carcinoma with virilization, and abdominal mass presented by Sipayya et al.,4 the palpable mass in this case due to is its size (11× 9×7 cm) while in the current case the size is (5×4×4cm). Regarding prognosis: good for both cases because the tumor-staging (II) with complete resection. Another case report of adrenocortical carcinoma: A two-year-old girl with features of cushings and virilization with metastasis to the lungs, presented by Gundgurthi A et al.,5 prognosis was poor for: *pure virilizing carcinomas, in general appear to have better prognosis (as in our case and Sipayya et al.,4 case) than other adrenal carcinomas,6 *the tumor’s stage was IV. Most of the adrenal tumors are sporadic; however, a fraction of them might be familial this supported by Mahloud JIM et al.,7 while in the current case and other cases mentioned above the family history was negative .Staging of Adrenocortical carcinoma in childhood varies from that in adults. Complete surgical resection is the only hope for long-term remission in these tumors. The staging involves the size, weight, and amount of resection of the tumor. Stage I is a tumor <5 cm, weighing <200 g, with complete resection; stage II ≥ 5 cm, > 200 g, with complete resection; stage III−local spread to lymph nodes, kidney, inferior vena cava or incomplete resection, and stage IV distant metastases to either lung or liver or to both. Seventy-five percent of the children present in stage I/II, 10% in stage III, and the remaining in stage IV. Surgery is the cornerstone of treatment in stages I-III of adrenocortical carcinoma, open surgery remains the gold standard and laparoscopic surgery is discouraged in view of excess locoregional recurrences.8
This case demonstrates some interesting features of adrenocortical carcinoma with unique pathologic findings presented with features of virilization. To our knowledge, this is the first case report in our country in this age group that attributed to increase awareness of physicians, patients and their families about endocrine disorders that necessitates more attention from high health authorities for endocrine centers and clinics.
None.
The author declares there is no conflict of interest.

©2015 Jumaili. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.