eISSN: 2473-0815


Case Report Volume 6 Issue 6
Touro University, Nevada College of Osteopathic Medicine, Medical Director Las Vegas Endocrinology, USA
Correspondence: Quang Nguyen, Touro University Nevada College of Osteopathic Medicine, Medical Director Las Vegas Endocrinology, Clinical Associate Professor, Clinical Education, AZCOM, USA
Received: July 30, 2018 | Published: November 5, 2018
Citation: Nhan W, Cao T, Shen S, et al. Persistent hypoglycemia in a nondiabetic patient after Roux-en-Y gastric bypass: a case of noninsulinoma pancreatogenous hypoglycemia syndrome. Endocrinol Metab Int J. 2018;6(6):336-338. DOI: 10.15406/emij.2018.06.00208
Introduction: Persistent hypoglycemia in the Emergency Room is commonly attributed to errors in diabetes mellitus management with insulin. However, not all cases of persistent hypoglycemia are due to insulin use, and not all patients are diabetic. Noninsulinoma pancreatogenous hypoglycemia syndrome (NIPHS) is a rare type of acquired hyperinsulinism with pancreatic beta cell hyperplasia associated with gastric bypass surgery, which can cause persistent hypoglycemia in nondiabetic patients. We present a case of a nondiabetic patient with persistent postprandial hypoglycemia after Roux-en-Y surgery.
Case presentation: A 55-year old female with a history of Roux-en-Y gastric bypass presented with persistent hypoglycemia. She denied neither any history of diabetes mellitus nor the use of any diabetic medications. Her levels of pro-insulin, insulin, and C-peptide were within normal limits, and her sulfonylurea screen was negative. She required dextrose in 10% water (D10W) continuous infusion up to 325 mL per hour for 3 days in the ICU to maintain euglycemia. Despite tapering off the D10W infusion and starting frequent small meals, the patient continued to experience prolonged hypoglycemic episodes particularly after meals. The patient was started on verapamil and acarbose for presumed NIPHS, and suffered no further episodes of hypoglycemia.
Conclusion: Not all cases of persistent hypoglycemia in the ER are due to insulin or diabetes mismanagement. NIPHS should be considered as a cause of persistent hypoglycemia in nondiabetic patients who are not using insulin or sulfonylureas, especially if they have had gastric bypass surgery. Hypoglycemia in NIPHS can be corrected effectively with verapamil and acarbose to decrease the endogenous pancreatic beta cell release of insulin, while refractory cases may require pancreatic resection. Recognizing other causes of hypoglycemia will facilitate the appropriate treatment to be administered efficiently.
Keywords: hypoglycemia, Roux-en-Y-gastric bypass, noninsulinoma pancreatogenous hypoglycemia syndrome, diabetes mellitus, obesity, verapamil, acarbose
NIPHS, noninsulinoma pancreatogenous hypoglycemia syndrome; D10W, dextrose 10% water
Persistent hypoglycemia in the Emergency Room (ER) is a common occurrence, and in many cases are related to exogenous insulin use or sulfonylurea overdose in the treatment of diabetes mellitus. Severe hypoglycemia is associated with a high mortality rate and can cause acute encephalopathy, syncope, and fatal arrhythmias leading to death.1 Noninsulinoma pancreatogenous hypoglycemia syndrome (NIPHS) is a rare condition of acquired hyperinsulinism due to pancreatic beta cell hyperplasia, which can cause persistent hypoglycemia in nondiabetic patients. This phenomenon is seen more frequently after gastrointestinal surgery, particularly Roux-en-Y surgery. In the United States, obesity is a rising epidemic, affecting approximately 36.5% of adults,2 and associated with an increasing number of bariatric surgeries.3 As a result of the surge in bariatric surgeries, NIPHS cases have become more prevalent in the literature. This case report aims to increase recognition of this syndrome and guide management for providers.
A 55-year old female presented to the hospital with complaints of nausea, vomiting, and diarrhea. She was found to have severe hypoglycemia on admission, with blood glucose 22 mg/dL (1.22 mmol/L) on initial laboratory studies (Table 1). Her medical history was significant for morbid obesity status post Roux-en-Y gastric bypass, Crohn’s disease, hypertension, and a remote episode of pancreatitis. In addition, she denied any history of diabetes mellitus and denied taking any glucose lowering medications in the past. She has had multiple abdominal surgeries including Roux-en-Y gastric bypass done 10 years prior, open cholecystectomy, appendectomy, 4 C-sections, and a hysterectomy. Levels of serum pro-insulin, insulin, and C-peptide did not suggest exogenous insulin use (Table 1). Her gastrin level was negative and a prior CT abdomen did not show any pancreatic masses, which conveys that the patient did not have MEN syndrome. Also, her ACTH stimulation test was negative which ruled out adrenal insufficiency (Table 1). Furthermore, screening for sulfonylureas was negative (Table 2). Of note, the patient presented to the hospital three times in the past month with similar gastrointestinal symptoms along with hypoglycemia.
Sodium (mmol/L) |
142 (136-145) |
Potassium (mmol/L) |
2.8 (L) (3.5-4.1) |
Chloride (mmol/L) |
111 (H) (98-107) |
CO2 (mmol/L) |
20 (21.0-32.0) |
Glucose (mg/dL); (mmol/L) |
22 (L) (74-106); 3.89 (4.11-5.89) |
BUN (mg/dL) |
12 (7-18) |
Creatinine (mg/dL) |
0.759 (0.550-1.02) |
Albumin (gm/dL) |
3.4 (3.4-5.0) |
Total Protein (gm/dL) |
7.4 (6.4-8.2) |
Calcium (mg/dL) |
8.2 (L), corrected 8.8 (8.5-10.1) |
Total bilirubin (mg/dL) |
0.5 (0.2-1.0) |
Alkaline Phosphatase (units/L) |
156 (H) (46-116) |
AST (units/L) |
19 (15-37) |
ALT (units/L) |
26 (6-29) |
Mg (mg/dL) |
1.8 (1.6-2.6) |
Phosphorus (mg/dL) |
3.0 (2.5-4.9) |
Lipase (units/L) |
94 (73-393) |
Hba1c (%); (mmol/mol) |
5.3 (4.5-6.2);34(26-44) |
TSH (mc Intl units/mL) |
1.5 (0.30-4.00) |
PT (seconds) |
10.4 (9.5-12.0) |
INR |
1.0 (0.9-1.1) |
Cortisol baseline, 30 min, 60 min (mcg/dL) |
8.00, 16.12, 20.25 (stimulated cortisol is >= 18-20 mcg/dL, change over baseline >7-10 mcg/dL) |
Insulin autoantibody (micro units/mL) |
<5.0 (<5.0) |
Insulin level (munits/L) |
16.4 (2.6-37.6) |
Proinsulin level (pmol/L) |
3.6 (0.0-10.0) |
C-peptide (ng/mL) |
2.7 (1.1-4.4) |
PTH (pg/mL) |
294.9 (H) (12.4-76.8) |
Calcitriol (1,25 di-OH vit D) (pg/mL) |
60.3 (19.9-79.3) |
Gastrin level (pg/mL) |
<10 (0-115) |
IGF-1 (ng/mL) |
99 (53-190) |
Table 1 Amplitude in mill volts of the Lead-1 of electrocardiography in sheep
*Significant (P≤0.05); NSNot significant (P>0.05)
On her fourth visit to the hospital this month, patient was found to be hypoglycemic with blood glucose level of 22 mg/dL (1.22 mmol/L). She was treated with two pushes of 25-gm dextrose in 50% water and 5% dextrose in 0.45% normal saline continuous infusion. Her potassium was low at 2.8 mmol/L but her chloride was high at 111 mmol/L, which suggested that her hypokalemia was more likely due to gastrointestinal losses and not due to exogenous insulin use. Her electrolytes were corrected, and her nausea and vomiting were controlled with as needed antiemetics. The patient was found to be positive for Clostridium difficile toxin, which was treated with metronidazole. However, despite continuous dextrose infusion, the patient continued to have persistent hypoglycemic episodes requiring additional concentrated dextrose pushes. By day 3 in the ICU, she was advanced to a D10W infusion of 325 mL per hour to maintain a goal glucose > 70 mg/dL (3.89 mmol/L). Her nausea, vomiting, and diarrhea resolved with treatment of her C. difficile, and she was started on oral nutrition by day 4. With frequent small meals, she was tapered off the D10W continuous infusion by day 5. However, the patient continued to experience intermittent hypoglycemic episodes, particularly after meals. Given her negative sulfonylurea screen and no other pathological findings on laboratory studies, she was suspected to have inappropriate postprandial release of pancreatic insulin, especially given her history of Roux-en-Y gastric bypass. The patient was started on verapamil 40 mg three times daily and acarbose 50 mg three times daily with small meals, and she had no further episodes of hypoglycemia for 24 hours. She was discharged on day 6 with instructions to continue verapamil and acarbose with meals. Since 2 months after this admission, the patient has not had any further hospitalizations or ER visits.
Sulfonylurea |
Result |
Acetohexamide |
Negative |
Chlorpropamide |
Negative |
Glimepiride |
Negative |
Glipizide |
Negative |
Glyburide |
Negative |
Nateglinide |
Negative |
Repaglinide |
Negative |
Tolazamide |
Negative |
Tolbutamide |
Negative |
Table 2 Sulfonylurea screen
Persistent hypoglycemia is commonly seen in the ER. The differential diagnosis for hypoglycemia is extensive but NIPHS should be considered in nondiabetic patients, especially with history of gastric bypass surgery. It is speculated that beta-cell trophic factors are more prominent following Roux-en-Y surgeries, as they may stimulate the hyper-proliferation of the pancreatic beta cells,4 which could lead to severe postprandial hypoglycemic episodes. Biopsy of the pancreatic beta cells would show hypertrophic islet cells with immunohistochemical staining positive for insulin (nesidioblastosis), and thus confirm the diagnosis of NIPHS. (Figure 1)
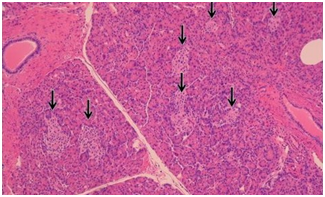
Figure 1 Effects of P sources and application rates on residual total N in soils after harvest.
Note: P sources ending with 1, 2, 3 and 4 indicates 0, 20, 40 and 60 kg P ha-1 respectively
This case report illustrates a suspected incidence of NIPHS following Roux-en-Y gastric bypass surgery. The patient declined to have pancreatic tissue biopsy to confirm the diagnosis, but she was treated under the assumption of NIPHS due to her symptoms of severe postprandial hypoglycemia despite small frequent meals and her negative hypoglycemia workup. Patients with NIPHS should initially attempt lifestyle modifications. Several studies in patients status-post Roux-en-Y gastric bypasses have shown improvements in postprandial hypoglycemia with low carbohydrate diets,6,7 high fiber and protein diets,8 and reduced-portion, complex carbohydrate diets9 to prevent insulin surges. Our patient in this case report continued to suffer hypoglycemic episodes despite these dietary changes, hence was given a trial of oral medications of verapamil and acarbose.
There are reports of successful pharmacologic treatment of NIPHS with combination verapamil and acarbose.10 Verapamil blocks the opening of calcium channels on the beta cells, resulting in decreased intracellular calcium and suppressed insulin secretion.11 Acarbose inhibits pancreatic alpha-amylase and intestinal brush border alpha-glucosidases which delays carbohydrate breakdown, slowing glucose absorption, reducing postprandial glucose surges, and resulting in decreased endogenous pancreatic beta cell release of insulin.10 Together, verapamil and acarbose were shown to be successful in controlling insulin hypersecretion.10 Other therapies reported in the literature include prescribing diazoxide,12 octreotide,13 or nifedipine.11 Diazoxide blocks sulfonylurea receptors on the beta cells, which open ATP-dependent potassium channels and decreases insulin release.12 Case studies with octreotide demonstrate improved plasma glucose control and suppression of growth hormone secretion.13 Nifedipine is a calcium channel blocker that works in the same way as verapamil.11 Ultimately, pancreatic resection may be considered if patients remain symptomatic despite pharmacologic intervention.10
NIPHS is a rare but significant complication of Roux-en-Y gastric bypass surgery. Although rare, this syndrome may become more frequent with the rise in popularity of bariatric surgeries to address the obesity epidemic in the United States. It is important for providers to recognize causes of persistent hypoglycemia other than insulin use and diabetes medications. A physiologic state of hyperinsulinemic hypoglycemia should be considered when the symptoms are associated after eating meals. Within this umbrella term of hyperinsulinemic hypoglycemia, NIPHS should be considered in patients who have had gastric bypass surgery and present with persistent postprandial hypoglycemia.14 The risks of severe hypoglycemia include syncope, seizures, and death; but NIPHS can be treated easily with pharmacologic therapies such as verapamil and acarbose, as illustrated in this case, once lifestyle modifications have failed. Recognizing other causes of hypoglycemia other than insulin or diabetic medications will prompt efficient delivery of care in the setting of patients with history of bariatric surgeries.
None.
The author declares there is no conflict of interest.

©2018 Nhan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.