eISSN: 2473-0815


Introduction: Acromegaly is a rare, chronic, insidious disease characterized by overproduction of growth hormone (GH) and its tissue mediator insulin-like growth factor 1 (IGF-I) typically from a pituitary adenoma. Recurrent acromegaly is established by GH hyper secretion after initial biochemical cure, and is even rarer than the disease itself, reported in only 2 to 3% of the cases.
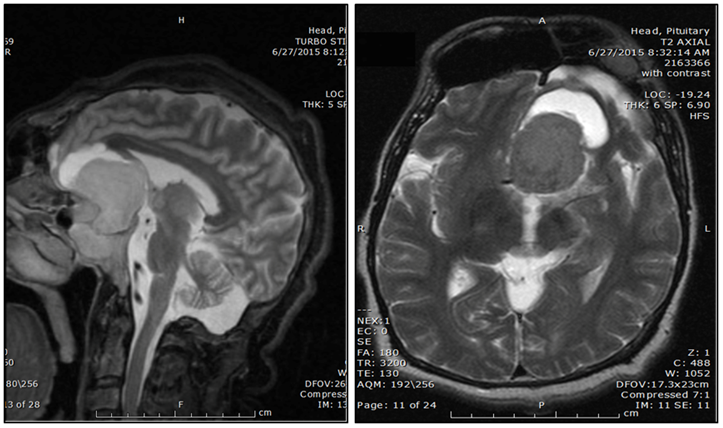
Case report: We present a case of a 44 year-old Hispanic male with a past medical history of acromegaly diagnosed 20 years ago initially treated with transsphenoidal microsurgery and open brain surgery two years after the first procedure. He was lost to follow up and presented to our outpatient clinic 18 years later complaining of frequent headaches with nose and hands enlargement. Physical examination revealed an overweight male patient with a height of 75 inches, enlarged nose, lips, splayed teeth, coarse facial features, macroglossia, enlargement of both hands with hyperhidrosis of his palms. Laboratory work up confirmed the diagnosis of recurrent acromegaly with elevated fasting IGF-I level. MRI of the brain showed a 4.3 x 3.8 cm pituitary macroadenoma with extensive suprasellar extension and optic chiasm compression.
Medical treatment with Octreotide Long-Acting Release(LAR) was started immediately and subsequent repeat IGF-I levels have shown progressive improvement.
Discussion: This patient’s case of recurrent acromegaly shows the importance of follow up after any surgical or medical intervention in acromegaly patients. Recurrence, though infrequent, is possible and these patients have been identified as a subset of patients that can be difficult to manage. Therefore close monitoring with IGF-I and GH levels is crucial to diagnose and treat recurrence of the disease and its comorbidities. Our goal was to achieve a biochemical cure, however given the fact that the patient refused any surgical intervention, makes the case even harder to manage. Somatostatin analogues have proven to be effective in cases like ours, yet its efficacy varies among studies.
Keywords: acromegaly; transsphenoidal; octreotide; hyperhidrosis; macroadenoma; transaminases
Acromegaly is an insidious disease characterized by overproduction of growth hormone (GH) and its tissue mediator insulin-like growth factor1 (IGF-I) typically from a pituitary adenoma.1 Approximately 3 to 4 cases of acromegaly per million population are newly diagnosed every year, with a prevalence of 5 to 6 cases per 100,000 population, which makes the disease very uncommon.1,2
The definition of cure of acromegaly is given by biochemical criteria that must be met in order to establish and confirm the control of the disease.
Recurrent acromegaly is determined by overproduction of GH after biochemical cure, and is even rarer than the disease itself, reported in only 2 to 3% of the cases.1 On the other hand, persistence of the disease is usually established after a consistently elevated GH level following a surgical excision of the adenoma. In this article we present a case of recurrent acromegaly and its medical management.
We present a case of a 44 year-old Hispanic male with a past medical history of acromegaly diagnosed 20 years ago. He was initially treated with transsphenoidal microsurgery in 1995 and open brain surgery in 1997.
He was lost to follow up and presented to our outpatient clinic 18 years later complaining of frequent headaches with nose and hands enlargement. Further questioning revealed that he was also having significant debilitating lower back pain, decreased left sided vision and erectile dysfunction. These symptoms were impairing his daily activities and social life, to an extent that he would avoid any exposure to friends or family. Even though he did notice some changes to his face, they occurred gradually and only noticed them when they were very obvious.
Physical examination revealed an overweight male with a BMI of 29.2 Kg/m2, height of 180cm (71 inches), enlarged nose, lips, splayed teeth, coarse facial features (Figure 1), macroglossia, enlargement of both hands (Figure 2) and hyperhidrosis of his palms. Ophthalmologic evaluation revealed left nasal hemianopia.
Laboratory work up confirmed the diagnosis of recurrent acromegaly with high fasting IGF-I level of 833ng/mL (52-328ng/mL).
MRI of the brain (Figure 3) showed a 4.3 x 3.8 cm pituitary macroadenoma with extensive suprasellar extension and optic chiasm compression. He was evaluated by neurosurgery, but the patient refused any surgical intervention.
Medical treatment with Octreotide Long-Acting Release (LAR) 30mg every four weeks was started immediately. After the second dose, the patient reported improvement of his back pain and decreased hyperhidrosis.
A repeat IGF-I level after 2 months of therapy was 826ng/mL (52-328ng/mL) and 542ng/mL (52-328ng/mL) after 5 months of therapy. Transaminases levels were also evaluated, which resulted normal with a normal Glutamic Oxalate-GOT (AST) of 24 U/L (15-41 U/L), Glutamic Pyruvic Transaminase (ALT) of 18 U/L (17-63 U/L) and Alkaline Phosphatase of 112 U/L (38-126 U/L).Even though his symptoms were still present during his last follow up visit, the patient had been able to tolerate his daily activities at home.
Acromegaly is a rare disease commonly caused by a GH secreting pituitary adenoma, frequently a macroadenoma (>1cm).3 The management of acromegaly should be always dedicated to improve the quality of life, signs and symptoms of the disease.
The cure in acromegaly is mainly biochemical, indicated by normalization of GH below 2.5ug/L, GH suppression to 1ug/L during an Oral Glucose Tolerance Test (OGTT) and IGF-1 level normalization for age and gender.1 In some cases, despite of establishing the cure of the disease, recurrence or persistence is possible.
Transspenoidal microsurgery has been demonstrated to be an effective way to treat acromegalic patients, however rates of cure with surgery alone have been reported only to 60%.4 Thus at least 40% of patient will be diagnosed with either persistent disease or recurrence,1,4 and will require further medical or surgical intervention.
This particular patient presented as recurrent acromegaly after 18 years initial surgical treatment, with debilitating signs and symptoms of the disease. Transsphenoidal microsurgery remains the first line of treatment,1 butmany medical options including somatostatin analogues, dopamine agonists, growth hormone receptor antagonists are available either alone or in combination and radiation therapy is also available.
Somatostatin analogues remain first line medical therapy, especially for cases like ours, which have recurred after failed surgeries. However the efficacy of these agents varies among studies.1 In fact some studies have reported higher efficacy of Octreotide compared to Lanreotide in reducing GH and IGF-I levels.5
Given the fact that the patient refused any surgical intervention, made this case even more difficult to manage. In fact, multiple studies have failed to demonstrate the efficacy of a repeat surgery for persistent or recurrent acromegaly.6
One of the most important factor in determining success of surgery is the location of the tumor and the surgical target on the MRI,1 which sometimes will preclude any surgical intervention.
It is important to follow up acromegalic patients after any surgical or medical intervention, because recurrence, though infrequent, is possible and these patients have been identified as a subset of patients that can be difficult to manage. Therefore close monitoring with IGF-I and GH levels, as well as periodic pituitary MRI’s is crucial to diagnose and treat recurrence of the disease and its comorbidities.
None.
The author declares that there are no conflicts of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.