eISSN: 2378-315X


Research Article Volume 13 Issue 1
1 Academic director at Clinical Bupa Santiago, Head of the unit of oral and maxillofacial surgery at Clinical Bupa Santiago, Oral and Maxillofacial Surgeon Hospital Dr. Luis Calvo Mackenna, Santiago, Chile
2 Oral and Maxillofacial Surgeon at Clinica Bupa Santiago and Hospital Exequiel Gonzalez Cortes, Santiago, Chile
3 Oral and Maxillofacial Surgeon at Clinica Bupa Santiago, Hospital Exequiel Gonzalez Cortes, Mutual de seguridad and Hospital Dr. Luis Calvo Mackenna Santiago, Chile
4 Head of the unit of oral and maxillofacial surgery at Hospital Exequiel Gonzalez Cortes and Hospital Dr. Luis Calvo Mackenna Santiago, Program director of oral and maxillofacial surgery at Universidad Mayor, Chile
5 Head of the unit of oral and maxillofacial surgery at Hospital Militar de Santiago, Head of Operating Room Services and oral and maxillofacial surgeon at Hospital Dr. Luis Calvo Mackenna Santiago, Chile
Correspondence: Daniel Jerez DDS, MSc, 1Academic director at Clinical Bupa Santiago, Head of the unit of oral and maxillofacial surgery at Clinical Bupa Santiago, Oral and Maxillofacial Surgeon Hospital Dr. Luis Calvo Mackenna, Santiago, Chile
Received: April 01, 2024 | Published: April 15, 2024
Citation: Daniel JDDS, German LDDS, Carlos FDDS, et al. Predictive factors of disc perforation of the temporomandibular joint (TMJ). Biom Biostat Int J. 2024;13(1):28-34. DOI: 10.15406/bbij.2024.13.00411
Magnetic resonance imaging (MRI) is the gold standard for diagnosing internal derangement, but its accuracy in detecting disc perforations varies. This cohort study included 92 patients who underwent arthroscopic surgery to identify associated variables. The presence of arthroscopically verified disc perforation served as the primary predictor variable, while the radiologist's diagnosis of disc perforation served as the primary outcome variable. Demographic data, patient signs, and symptoms were considered as covariates. Statistical tests were performed with a significance level of 5%. Logistic regression models were used to predict disc perforation, and diagnostic accuracy was assessed using ROC curves. Among 155 joints analyzed (92 patients: 135 females, 20 male), radiologists' MRI interpretations did not significantly correlate with verified disc perforation (p<0.218), showing 14.3% sensitivity and 92.5% specificity. Age, symptomatic onset, joint noise type, osteoarthritis diagnosis, altered disc shape, and Wilkes classification showed significant associations (p<0.05). A logistic regression model used associated variables for disc perforation. Risk factors: symptom onset time, joint crepitus, osteoarthrosis diagnosis by MRI; joint click as protective. The model demonstrated high diagnostic accuracy (AUC of 0.836, 95% CI_0.76–0.91). Radiologists' MRI interpretation was unreliable, but our model accurately predicted disc perforation. Identifying these factors could guide surgical decisions.
Keywords: TMJ surgery, TMJ arthroscopic surgery, disc perforation, discectomy
Temporomandibular disorders encompass a series of clinical entities that can affect the muscles and the temporomandibular joint (TMJ).1 After chronic low back pain, temporomandibular joint disorders are the second most common musculoskeletal condition,2–4 and it is estimated that they can affect between 5 and 30% of the North American population.3,5 Disc perforation, considered a degenerative state of the joint, is observed in the end stages of the disease. The incidence of disc perforation is reported between 5% and 15% of patients with disc displacement.6,7 This condition is relevant for the treatment plan since advanced stages of the joint disease require a more aggressive surgical approach (discectomy or joint replacement). Therefore, diagnostic precision is relevant in decision-making in managing this type of pathology.
The gold standard for diagnosing internal derangement (ID) is magnetic resonance imaging (MRI).3 MRIs detect disc position, disc shape, signs suggestive of synovitis, an approximation to the condylar bone state (osteoarthrosis, osteoarthritis), and disc perforations.1 The accuracy of MRI in the diagnosis of disc perforations is variable.8–12 Rao et al. reported an accuracy of only 3% for diagnosing disc perforations.8,9 Nevertheless, Shen et al. conducted a retrospective study including 2,524 joints that underwent arthroscopic surgery. The authors compared the operative findings of disc perforation, considering surgical exploration as the gold-standard diagnosis, with the pre-surgical MRI reports. The authors described a high level of precision measured with ROC curves with an area under the curve (AUC) of 0.808 (0.77, 0.85, p<0,05).12 The authors described an image acquisition protocol that increased the accuracy in diagnosing disc perforations, concluding that MRI is a reliable diagnostic technique for TMJ disc perforations.12
However, having the same MR protocol for all patients is complex and does not reflect the reality of the clinical routine. Usually, patients go to the imaging center, where their service provider gives them better coverage for the exam. Therefore, surgeons receive MRIs from different centers, informed by different radiologists and with different protocols, so, therefore, the reports and their interpretation may suffer from high variability. Due to this high variability in MRI interpretation, identifying imaging and clinical variables of disc perforation is essential for decision-making, given the prognosis and the different alternatives for managing this type of condition.
If the study based on resonances is unreliable, are there some preoperative and imaging variables that can predict the presence of fiscal perforation? We hypothesize that there are signs, symptoms, and imaging findings related to the TMJ's disc perforations. Our objectives are to 1: identify what MRI features correlate with disc perforation, 2: identify what preoperative variables correlate with disc perforation, and 3: create a predictive model to determine the presence of disc perforation.
This study corresponds to a retrospective case series, which included all consecutive patients who underwent arthroscopic TMJ surgery at Clínica Bupa Santiago from July 2020 to July 2022. The inclusion criteria were patients with chronic pain or dysfunction that has failed to respond to conventional non-invasive therapy, or due to preoperative tests or patient preferences, arthroscopic surgery was chosen as the first indication of therapy. Patients without complete preoperative data, TMJ-MRI images, radiologist reports (at least six weeks), and intraoperative data (video and operation notes) were excluded.
The study was approved by the scientific ethics committee of Clínica Bupa Santiago (No. Res. CEC CBS/01-2022) and followed all tenets of the Declaration of Helsinki for research involving human subjects. The data was obtained from the analysis of clinical records, radiological reports, images (pre-surgical MRI), a surgical protocol review, and arthroscopic surgery videos. Patients authorized the review of their clinical records through informed consent.
Our primary predictor variable was arthroscopically diagnosed disc perforation, which we confirmed throw surgical videos (Figure 1) and surgical operation notes. The video review of the surgery was performed by the co-author (GL), who corroborated the data obtained from the operation notes. If differences were between the operation notes and the video, it was decided to keep what was reviewed in the surgical video. The co-author (GL) was blinded to any information when he assessed the videos, so he had no information on the previous diagnosis of the images.
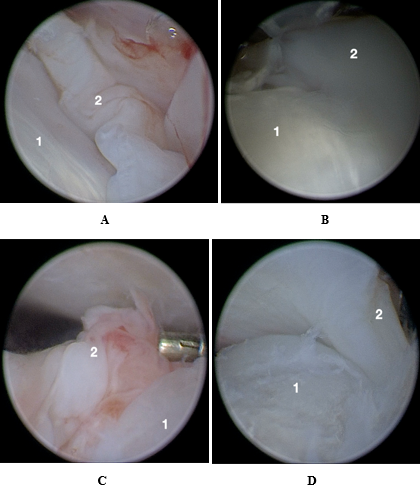
Figure 1 A Intraoperative photograph. Different presentation of arthroscopic diagnostic of disc perforation. 1= mandible condyle, 2= disc perforation.
The primary outcome variable was the radiologist's diagnosis of disc perforation. A bilateral TMJ MRI protocol was performed on each patient according to our protocol (sagittal sequences T1, T2, PD_Fse in occlusion and dynamic. Coronal sequences PD_Fse and T1). The images were acquired in a Siemens Magnetom Sola 1.5 Tesla MR scanner in the Clínica Bupa Santiago imaging service. The images were analyzed by the Clinica Bupa Santiago neuroradiology and maxillofacial radiology team, integrated up of a total of 4 specialists. From the assessment of the MR images and the radiologist's report, the following information was obtained, joint effusion, signs of osteoarthrosis/osteoarthritis, disc dislocation, disc reduction, altered disc shape, and if the disc shows signs of perforation. The surgeon interpreted the Wilkes classification from MRI images and preoperative clinical.
The secondary outcome variables were demographic data, anamnesis data, and signs and symptoms of the patient. Through an analysis of clinical records, the following information was obtained: age, gender, surgical side, cause of the disorder, time since the onset of symptoms (approximate in years), history of bruxism, medical therapy (NAIDS, pregabalin, muscle relaxants, others), history of conservative treatment (kinesiology, occlusal splint, intraarticular infiltrations, and arthrocentesis), maximum preoperative mouth opening, presence of preoperative noise, type of noise (click or crepitus) and postoperative pain (measured on a visual analog scale (VAS) from 0 to 10). Range of motion (maximum mouth opening) was measured with specific mouth opening measurement rulers (Sammons Preston Therabite, Patterson Medical Holdings Inc). The time since the onset of symptoms was measured and approximated in years. For those patients with evolution times of less than six months, a value of 0 was assigned. Those older than six months were assigned a value of 1. Those who reported time since onset of symptoms of more than 20 years were assigned a value of 20.
The data was incorporated into the SPSS program (IBM version 25) to perform the statistical analysis performed by the author (D.J). Descriptive statistics and an analysis of the association between preoperative variables and the intraoperative variable of the arthroscopically diagnosed disc perforation were performed.
Arthroscopic surgery was performed by the author (D.J), under general anesthesia, with an arthroscopy set with a 2.4 mm optic, a 3.2 mm protection sleeve (Karl Storz, Tuttlingen, Germany), and a video tower system (Karl Storz, Tuttlingen, Germany).
For this study, an alpha of 5% was set as the significance level. The statistical tests performed were the Chi2 or T-student test for independent samples appropriate to the variable type. Independent variables were tested for normal distribution with the Shapiro–Wilk test, and parametric tests were performed for those with normal distribution. The variables were classified according to categorical or continuous.
The accuracy of the interpretation of disc perforation through MRI, compared with the arthroscopically diagnosed disc perforation, was measured with likelihood ratios obtained throw sensibility and specificity. Also, the prediction of disc perforation was carried out using statistical models with logistic regression (forward-Wald method), including those variables that present significant levels of association with the arthroscopically diagnosed disc perforation. The model was applied to the entire sample to estimate the probability of disc perforation. From this probability, a ROC was constructed to assess the model's accuracy. From this model, a disc perforation score was constructed. The score was applied to the sample and to test the predictive level, and a ROC curve was drawn on the result.
Table I summarizes the descriptive statistics of preoperative and MRI variables. A total of 155 joints corresponding to 92 patients were analyzed. The average age was 28.9 years, ranging from 11 to 74 years. Of the total sample, 135 joints correspond to female patients (87.1%) and 20 to men (12.9%). Seventy-five joints corresponded to the right side (48.4%) and 80 to the left (51.6%). The leading identified cause of the disorder was a dentofacial anomaly (32.3%), followed by a history of mandibular trauma (11.6%), after dental treatment (6.5%), bruxism (3.9%), autoimmune pathology (5.2%), after orthognathic surgery (1.9%), overload (1.3%) and septic arthritis (0.6%). Most patients (36.8%) could not identify the disorder's cause. The average time since the onset of symptoms was 8.6. The maximum pre-surgical mouth opening was a mean of 31 mm. The average preoperative pain was six on VAS. Sixty-nine joints had no prior noise (44.5%), while 86 had noise (55.5%), of which 64 were click type. (17.8%) and 22 crepitus type (12.6%). Regarding previous treatment, a total of 133 joints received some type of pre-surgical medical treatment (87.4%), of which the most frequent was the use of NSAIDs (74.1%), followed using muscle relaxants (59, 8%) and the use of pregabalin (17.8%). A total of 98 joints (67.2%) had a history of conservative treatment before arthroscopic surgery, of which the most frequent was the use of occlusal splint (53.4%), arthrocentesis with medication infiltration (25.3%), kinesiology (20.7%), Botox infiltrations (7.5%) and prior joint surgery (0.6%). From the MRI report analysis, the main sign described was disc displacement which occurred in 143 joints (92.3%), of which 60 (41.9%) were reported with reduction and 83 (58.1%) without reduction. Joint effusion was the second most reported sign in the images, with a total of 138 joints (89%), followed by osteoarthrosis in 74 joints (47.7%). Seventy-one discs were reported with altered shape (45.8%), and only 14 had signs of perforation (9%). Regarding the Wilkes classification, two joints were classified as Wilkes I (1.3%), 35 as Wilkes II (22.6%), 40 as Wilkes III (25.8%), 53 as Wilkes IV (34, 2%), and 25 as Wilkes V (16.1%). From the intraoperative findings, it was observed that 144 joints presented disc displacement (92.9%), of which 55 reduced and 89 did not. 59 discs had shape alterations (38.1%), and 35 had disc perforations (22.6%). Of these 35 perforated discs, 18 (51.4%) were of a size that allowed repair. In contrast, 17 (48.6%) of them were not feasible to repair, in which arthroscopic discectomies were performed (11.1% of the total sample).
|
|
Variable name |
Mean (Range / SD) |
|
|
N: 155 joints, 92 patients |
Frequency (percentage) |
|
Preoperative variables |
Age |
28,9 yrs (11-74 yrs / 12,2 yrs) |
|
Maximum mouth opening |
31 mm (0-50 / 9,6 mm) |
|
|
Preoperative pain (VAS scale) |
6 (0-10 / 2,3) |
|
|
Time since symptom onset |
8,6 yrs (1-20 / 2,9 yrs) |
|
|
Sex |
||
Men |
20 (12,9%) |
|
Women |
135 (87,1%) |
|
|
Side |
||
Right |
75 (48,4%) |
|
Left |
80 (51.6%) |
|
|
Conservative treatment |
98 (67,2%) |
|
|
Noise presence |
86 (54.5%) |
|
|
Click |
64 (74,4%) |
|
|
Crepitus |
22 (25,6%) |
|
|
MRI variables |
||
|
Effusion |
138 (89%) |
|
|
Osteoarthrosis |
74 (47,7%) |
|
|
Disc displacement |
143 (92,3%) |
|
|
Disc reduction |
60 (42%) |
|
|
Disc shape alteration |
71 (45,8%) |
|
|
Disc perforation |
14 (9%) |
|
|
Wilkes Classification |
||
|
Wilkes I |
2 (1,3%) |
|
|
Wilkes II |
32 (22,6%) |
|
|
Wilkes III |
50 (25,8%) |
|
|
Wilkes IV |
53 (34,2%) |
|
|
Wilkes V |
25 (16,1%) |
|
|
Surgical variables |
||
|
Disc displacement |
144 (92,9%) |
|
|
Disc reduction |
55 (38,2%) |
|
|
Disc shape alteration |
59 (38,1%) |
|
|
|
Disc perforation |
35 (22,6%) |
Table 1 Descriptive statistic
Table 2 summarizes the association analysis between preoperative variables, MRI findings variables, and arthroscopically diagnosed disc perforation. Of the preoperative variables studied, the type of noise (click or crepitus) and the time since symptom onset measured in years showed a significant level of association with the outcome (disc perforation) (p<0.001). In contrast, age (p<0.309), maximum preoperative mouth opening (p<0.326), preoperative pain measured on the VAS scale (p<0.99), gender (p<0.767), side (p<0 .52), cause of the disorder (p<0.654) and presence of noise (p<0.319) did not show statistical significance. Furthermore, the history of having undergone previous conservative treatment did not show a significant value either (p<0.7). Of the findings described in the MRI, osteoarthrosis (p<0.001) and the description of disc shape alteration (p<0.002) showed a significant level of association with the disc perforation variable. On the other hand, effusion (p<0.184), disc dislocation (p<0.051), reduction (p<0.049), and the interpretation of disc perforation were not significant (p<0.218). The Wilkes classification showed a significant level of association with the disc perforation variable (p<0.001).
The reported sensitivity and specificity for the interpretation of disc perforation by the radiologist were 14.3% and 92.5 %, respectively. The positive likelihood rate (LR+) was 1.9, while the negative likelihood rate (LR-) was 0.93.
|
Covariate |
Not - perforated disc in MRI (n=141) |
Perforated disc in MRI (n=14) |
P-value |
||
|
Age (years) |
29,2 |
35,7 |
0,118 |
||
|
Maximum mouth opening |
30,2 |
33 |
0,41 |
||
|
Preoperative pain (VAS scale) |
6,3 |
6,7 |
0,56 |
||
|
Time since symptom onset |
4,3 |
5,6 |
0,18 |
||
|
Sex |
0,193 |
||||
Men |
11 |
0 |
|||
Women |
70 |
11 |
|||
|
Side |
0,563 |
||||
Right |
67 |
8 |
|||
Left |
74 |
6 |
|||
|
Conservative treatment |
90 |
8 |
0,903 |
||
|
Noise presence |
78 |
8 |
0,896 |
||
|
Click |
59 |
5 |
|||
|
Crepitus |
19 |
3 |
|||
|
MRI variables |
|||||
|
Effusion |
126 |
12 |
0,677 |
||
|
Osteoarthrosis |
62 |
12 |
0,003 |
||
|
Disc displacement |
129 |
14 |
0,256 |
||
|
Disc reduction |
57 |
3 |
0,124 |
||
|
Disc shape alteration |
57 |
14 |
<0.001 |
||
|
Wilkes Classification |
<0.001 |
||||
|
Wilkes I |
2 |
0 |
|||
|
Wilkes II |
35 |
0 |
|||
|
Wilkes III |
40 |
0 |
|||
|
Wilkes IV |
51 |
2 |
|||
|
Wilkes V |
13 |
12 |
|||
|
Surgical variables |
|||||
|
Disc displacement |
131 |
13 |
0,994 |
||
|
Disc reduction |
53 |
2 |
0,207 |
||
|
Disc shape alteration |
54 |
5 |
0,849 |
||
Table 2 Distribution of covariates by disc perforation in magnetic resonance imaging (MRI)
The risk variables included in the model were: osteoarthrosis, the presence of crepitus, and the time since the onset of symptoms. Instead, the only protective variable was the presence of joint click. The model's area under the curve (AUC) was 0.836 (95% CI 0,76 – 0,91). From this model, a score was constructed by adjusting the values. The adjusted disc perforation score model was Disc Perforation Score = 17*osteoarthrosis -3*joint click + 16*joint crepitus + 2* time since onset of symptoms. The score can be interpreted as the higher the value, the greater risk of disc perforation. The AUC of the score was 0.836 (95% CI 0,76 – 0,91) (Table 3-5) (Figure 2).
|
Covariate |
Not - perforated disc in Artroscopy (n=141) |
Perforated disc in Artroscopy (n=35) |
P-value |
|
Age (years) |
28,2 |
34,5 |
0,035 |
|
Maximum mouth opening |
31,2 |
29,5 |
0,45 |
|
Preoperative pain (VAS scale) |
6,3 |
6,5 |
0,78 |
|
Time since symptom onset |
3,8 |
6,3 |
0,001 |
|
Sex |
0,429 |
||
Men |
9 |
2 |
|
Women |
57 |
24 |
|
|
Side |
0,052 |
||
Right |
53 |
22 |
|
Left |
67 |
13 |
|
|
Conservative treatment |
75 |
23 |
0,729 |
|
Noise presence |
64 |
22 |
|
|
Click |
55 |
9 |
|
|
Crepitus |
9 |
13 |
|
|
MRI variables |
|||
|
Effusion |
109 |
29 |
0,184 |
|
Osteoarthrosis |
46 |
28 |
<0.001 |
|
Disc displacement |
108 |
35 |
0,051 |
|
Disc reduction |
49 |
11 |
0,049 |
|
Disc shape alteration |
47 |
24 |
0,002 |
|
Wilkes Classification |
<0.001 |
||
|
Wilkes I |
2 |
0 |
|
|
Wilkes II |
35 |
0 |
|
|
Wilkes III |
33 |
7 |
|
|
Wilkes IV |
38 |
15 |
|
|
Wilkes V |
12 |
13 |
|
|
Surgical variables |
|||
|
Disc displacement |
110 |
34 |
0,627 |
|
Disc reduction |
50 |
5 |
|
|
Disc shape alteration |
31 |
28 |
<0.001 |
Table 3 Distribution of covariates by disc perforation in arthroscopy
|
|
|
Arthroscopic disc perforation |
||
|
+ |
- |
Total |
||
|
Predicted disc perforation |
+ |
14 |
6 |
20 |
|
- |
21 |
114 |
135 |
|
|
|
Total |
35 |
120 |
155 |
|
Covariates |
Odds ratio |
95% confidence interval |
|
|
Time since onset of symptoms |
1,22 |
1.055025-1.420266 |
|
|
Click |
0,72 |
.2635474-1.963449 |
|
|
Crepitus |
5,01 |
1.508458-16.61426 |
|
|
Osteoarthrosis |
5,34 |
2.008327-14.19214 |
|
Table 5 The adjusted disc perforation score model was Disc Perforation Score = 17*osteoarthrosis -3*joint click + 16*joint crepitus + 2* time since onset of symptoms
Although MRI is considered the gold standard for the diagnosis of TMJ ID, the evidence is not conclusive regarding the role of this image in identifying and measuring the size of disc perforations.12–14 In our series of patients, the radiologist's interpretation of the presence of disc perforations showed a low diagnostic accuracy (LR+ of 1.9 and LR- of 0.93). However, the study of preoperative variables and imaging findings would allow disc perforation to be predicted with a high percentage of accuracy. Of the variables analyzed, age, time since symptom onset, type of joint noise (click or crepitus) and imaging diagnosis of osteoarthritis, altered disc shape, and the Wilkes classification showed a significant association with the confirmation of intra-articular disc perforation (Table 2). To reduce bias, a regression model was conducted. The risk variables included in the model were the time since the onset of symptoms (the longer the time, the greater the risk of perforation), the presence of joint crepitus, and the diagnosis of osteoarthrosis by MRI study. In contrast, the presence of an articular click proved to be a protective factor for disc perforation. To test the predictive level of the model, the score was applied to the sample, and a ROC curve was drawn on the result (Figure 2). The area under the curve showed the same predictive level as the model (0.836, 95% CI 0,76 – 0,91). The presence of joint noise is a sign of joint disease. The click is generally considered an initial and intermediate state of the pathology. However, crepitus is considered an advanced sign of joint pathology. The patient refers to this type of noise as the presence of "sand or glass" inside the joint. Theoretically, joint noises are caused in the presence of perforations by the friction that occurs between the head of the mandibular condyle and the glenoid fossa. The time since the onset of symptoms showed a high association with disc perforation. It should be noted that the Wilkes classification7 showed a significant level of association with the disc perforation variable (p<0.001). Except for the time since the onset of symptoms, the other variables included in the score (osteoarthrosis, joint click, and joint crepitus) are present in the Wilkes classification. This further validates the application of this classification for decision-making in TMJ surgical pathology.
By consensus, the patient with ID usually begins with conservative treatments (NSAIDs, occlusal splints, physiotherapy, infiltrations, and arthrocentesis.). This approach can cause patients to remain in non-invasive treatments for a long time, increasing the risk of chronicity and, according to the results of this study, increasing the possibility of generating disc perforation. The evidence and the current trend are to avoid postponing the indication for surgery.15,16 Also, it is even postulated that arthroscopic surgery could be indicated as the first line of treatment,15 which generates a paradigm shift with the dogma that conservative treatment should always be the first line of treatment, and surgery should be proposed if it fails. Tran et al. reviewed systematic reviews and clinical guidelines for ID treatment published in the last 5 and 10 years, respectively.16 The authors conclude that conservative treatments should last not more than three months, and if the patient does not show improvement, intra-articular treatment (arthrocentesis or arthroscopy) should be indicated.16 In our series of patients, the mean time since the onset of symptoms was 8.6 years, and 67.2% had some type of previous conservative treatment. So, in our case, patients were in conservative treatment for a long time, increasing the risk of generating irreversible degenerative pathology.
Regarding treatment, there is consensus that the treatment of disc perforations is performed by open surgery, performing repair (when size allows), discectomy (with or without replacement), or joint replacement.17 However, there is current evidence of good results with minimally invasive surgical management using arthroscopic surgery.18,19 Quinn and Stover describe positive results with level I arthroscopy (lysis and lavage) and remodeling of the perforation margins. Their study consisted of 44 joints treated in 25 patients followed up for an average of 40.8 months, of which 29 had disc perforations. The surgery included 14 abrasive arthroplasties and 24 motorized or Holmium laser arthroplasties.18 The authors demonstrated an improvement in mouth opening and pain reduction, concluding that this procedure can replace open discectomy in case of perforations.18 In contrast, Liu et al. reported a series of 112 patients (135 joints) who underwent disc perforation closure with arthroscopic surgery (Yang's technique).19 The reported success rate at the 12-month follow-up was 90.4%.19 Although they show excellent results, this success rate is lower than that of patients undergoing the same surgery without disc perforation (success rate of 95.4%).20–22 This difference is expected due to the degenerative state in which a joint is found when the disc is perforated, further confirming the importance of early treatment in suspected perforations. It should also be considered that the arthroscopic technique reported by the authors (Yang's technique) is considered the most stable20 but simultaneously the most complex to perform. This requires personalized instruments, making access to it more difficult.20 However, in a technical report published by the author (D.J), a modification was described to perform it without requiring these types of personalized instruments (23). In our series of patients, 35 joints presented disc perforation, of which 18 underwent disc repair using Yang's technique (51.4%). In contrast, 17 (48.6%) underwent arthroscopic discectomy (11.1% of the total sample). Our discectomy technique uses two working portals, a coblation probe (coblator II, Smith and Nephew, Andover, MA, USA) and Radius 2.0 motorized shaver. The evolution of both and the description of the surgical technique are outside the scope of this work and will be described in a separate study.
The study suffered from some limitations. We performed a retrospective case series, which may introduce bias to the results. Patients self-report the onset of symptoms reducing the reliability of this variable. Another drawback of this study is that different radiologists interpreted the MRIs, which could lead to inconsistent radiological reports. Although this concerns the authors, having reports from different radiologists represents the reality of our daily practice. Nevertheless, this study is a valuable starting point for evaluating more reliable disc perforation methods.
In conclusion, our series of patients showed that the interpretation of MRI is unreliable in determining the presence of disc perforations; therefore, identifying these factors before the treatment decision would allow the surgeon to change the surgical indication according to skills and tools. In addition, this confirms that diagnostic arthroscopy (first puncture or level I) should be considered the gold-standard diagnosis of intra-articular pathology.10 Nevertheless, our model allows us to identify predictive variables of disc perforation with high diagnostic accuracy. Identifying these factors before the treatment decision would allow the surgeon to change the surgical indication according to his preferences and, in turn, improve the prognosis of joint disease. Also, arthroscopic surgery could be indicated as the first line of treatment,15 which generates a paradigm shift with the dogma that conservative treatment should always be the first line of treatment, and surgery should be proposed if it fails.
None.
The authors declare there is not any conflict of interest.
None.

©2024 Daniel, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
2 7