Advances in
eISSN: 2572-8490


Review Article Volume 4 Issue 3
General Director of Modern Computer Medical Technology LLC, Russia
Correspondence: Moscow L Klukin, General Director of Modern Computer Medical Technology LLC, Honorary Academician of the Russian Academy of Medical Sciences, Honored Inventor of the Russian Federation, Russia
Received: April 09, 2018 | Published: May 9, 2018
Citation: Klukin ML. DOT device as absolutely safe and ergonomic tool for diagnosing breast cancer and monitoring the dynamics of development or rehabilitation of this disease. Adv Tissue Eng Regen Med Open Access. 2018;4(3):43–46. DOI: 10.15406/atroa.2018.04.00076
The paper discusses topical results on early and absolutely safe diagnosis of breast cancer with the help of the domestic DOT apparatus. It is shown that in the prevention of breast cancer at the preclinical stage of the development of this disease with the help of DOT it becomes possible to apply artificial intelligence for its timely detection. Using an array of thermal examination data, the patient's MF allows for an effective choice of treatment strategy by selecting optimal therapy at this stage of breast cancer development.
DOT, thermal volumetric tomograph; CM, conventional methods widely used in the clinic now; CT, computer tomograph; MRI, magnetic resonance tomograph; US, ultrasound sonar; RM, X-ray mammograph; PET-CT, positron- emission diagnostics; MG, mammary gland; Br, bra equipped with a matrix of thermal sensors; DT, remote thermal imager; CrT, cancer tumor; BT, benign tumor; BC, breast cancer; TD, time of doubling cancer cells; PT, some form or a tumor pathology
The creator of the national mammology, academician of the RAN, professor L. Lindenbraten with co-authors in 1997 expressed the criteria for a successful solution to the problem of breast cancer: - "the timely detection of breast cancer ensures the preservation of the life of the female population. Organ-saving treatments and reducing the cost of diagnosis and therapy are essential. National and regional programs of mass screening examinations, creation of Federal and regional registers of persons who underwent screening and patients with breast cancer are necessary".1 However, these criteria are not implemented in the current clinic due to the presence of radiation methods in service of medicine: ultrasound (sonar), CT, MRI, PM, PET-CT, which do not provide early and safe diagnosis.2,3
CrT as a tumor means the presence of an area in which the internal volume differs from the surrounding tissues in the normal MG (in structure or thermophysical properties). This is used as a diagnosis with the use of radial CM methods, which are delayed for a long time in comparison with when a tumor is detected at an early, preclinical stage. Breast cancer begins with the division of mutated cell. As the number of these cells increases in the place of their localization there is heating in this place and, accordingly, disturbed metabolism. Pre-clinical stage lasts until the moment when the СM has already fixed CrT. Until then, the patient does not feel the tumor due to the lack of pain symptoms. Assuming that the time of the development cycle of breast cancer from the appearance of the first cancer cell to the lethal outcome ends when the diameter of the CrT is reached in 100 mm, three quarters of this time is preclinical, in which metastases do not yet occur.4 Therefore, if CrT is detected at the preclinical stage, it is much easier to destroy it by selection of therapy provided if the screening is safe, allowing the dynamics to observe degradation of the tumor, and this causes a lower cost of treatment.
The PET-CT method works in the preclinical stage, but it has two drawbacks: a) it is dangerous because the patient is given a radioactive agent into the mammary gland, and the fact that this organ has increased radio sensitivity is provoked by a new tumor and b) it is accompanied by high costs and deficit expensive equipment.
To date, there have been publications and patents on the development of new means of "early" detection of breast cancer, which are based on the use of templates of temperature sensors built into the elastic Br (made from tissue or latex).5–7 Such bras are designed to detect breast cancer if they are worn for hours or even days by screening the disease. Their inherent property is the sharply increased inertia of the temperature sensors, which reduces their temperature sensitivity and distorts the heat exchange mode of the MG due to the inserted layer of material between MG and the environment, which in turn leads to increased sweating. However, the decisive factor for the inapplicability of such products is the ignoring of the newly discovered effect of non-stationary thermal relief in the breasts with a relatively high frequenc,8 which ensures the levelling of the survey results due to the longer duration of thermal exposure compared with the rate of change of the said temperature relief on the skin of the breast (white noise from temperature traces).
In this way the primary factors for the success of curing breast cancer is in a survey technique that is absolutely safe and provides rapid detection of the disease at a preclinical level. These requirements for diagnostic equipment not only allow sufficient time for the success of the cure, but also provide an opportunity to quickly observe the dynamics of treatment, and therefore, during screening, to ensure the selection of optimal therapy during treatment or in the rehabilitation of this disease. Such a technique is the DOT method.
The theoretical basis and principles of using the DOT-technique in the clinic is based on the detection of diseases in the human body by scanning the MG skin temperature with a temperature sensor with an error of the order of 10-3°C, placed in the autonomous and portable head of the device. Scanning is performed through regular openings in a bra that is worn on the chests, on both MGs. The time of examination lasts depending on the size of the bust from 5 to 8 minutes, after which the measurements are transferred to the computer via the cable. After processing on the computer, the monitor displays the mammograms in color with a two-dimensional relief of the temperature gradients on the skin of the MGs, either in "normal" or with CrT. These gradients reflect the results of the perturbation of the patient's internal heat flux due to interference by any form of pathology tumor. In this case, the tumor is modeled by a small body placed in a half-space at some distance from its surface (Figure 1).
For the first time, the solution of the problem of detecting a small body in a half-space of a solid medium with a constant heat flux from inside which is scattered from its boundary by convection into an atmosphere with a fixed temperature was published in.9 Later, it was proposed to be developed and tested in a clinic for a similar solution for a warm-blooded subject in.10–17
In the clinic, a similar model, where the software in the form of breast cancer, caused by the appearance and growth of cancer cells in the mammary glands was examined for a large base (85,000 patients) by professor M. Gautherie (Pasteur Institute, France). These examinations were conducted with the purpose of studying the parameters of the development of breast cancer by immersing a thin needle - a thermocouple into a tumor. The temperature was measured by a thermocouple and the immersion coordinates were monitored by x-ray.18 The volume of studies conducted and the reliability of the data make it possible to use the results obtained by M. Gautherie in the DOT method as safer, more rapid and ergonomic, since CMs currently do not provide the costs and diagnostic value of the breast cancer clinic - they are dangerous19,20 is not recommended until the age of patients at 40 years21 in contrast to DOT, which is recommended by the Ministry of Health of Russia for the examination of MG patients of any age and for work in the preclinical stage of breast cancer, where it does not give false positive sludge false negative readings.22
The results of DOT-surveys combined with subsequent digital processing on a computer can be compared with a tomogram, but with a smaller spatial resolution due to the thermal model, but they are suitable for work at the preclinical stage of breast cancer, which makes it possible to work out adequate therapy for any age of the patient.
Previously, it was shown that the time of doubling the cells of a particular patient (TD) in BC is unchanged during the disease of breast cancer and varies individually from a few weeks to 400 days.23,24 The growth of CrT is characterized by an exponential, starting with the appearance of a cancer cell, a diameter of about 10 μm and, accordingly, this law describes the regularity (1)
(1)
where Vt is a finite volume of CrT, V0 - is its initial volume, and nt is the number of cell divisions. The growth of tumor volume depends on the time t, the doubling time TD is individual. Figure 2 shows the growth curves of CrT for two values of TD in curves A and B.
It follows from (1) that the volume of PO depending on t can be determined as
(2)
where k is the exponent constant. From (2) with Ds=10 cm (lethal size of Crt) , it follows thatThe main meaning of the diagram in Figure 2 is the possibility of using the merits of the DOT method as completely safe in the diagnosis of MG at the preclinical stage of breast cancer, indicated in Figure 2 in the range of DS values from 0.3 cm to 0.5 cm, allowing screening with any reasonable frequency,2 in order to avoid the masking effect of the non-stationary nature of the temperature gradient field.8 The peculiarity of this approach is the consideration of the nature of heat exchange at the preclinical stage, when the pronounced metastasis process does not yet take place and the tumor retains its coordinates. As the CrT grows, the screening reveals the degradation of the heat flux maximum in terms of the intensity of the positive temperature gradient, as shown in Figure 3.
The peculiarity of this approach is the use of the result of the analysis of the evaluation of the connection of the cutaneous projection of the gradient with the invariant coordinate of the depth of the tumor center10
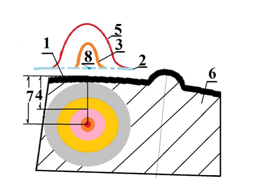
Figure 3 Scheme of the formation of the change in the relief of the temperature field on the skin of the MG at the growth of CrT: 1 - the skin of MG, 2 - the temperature of the MG in the norm, 3 - the relief with an intermediate CrT size 4, 5 - the relief with the minimal CrT 7, 6- tissue in norm, 8- relief at a finite tumor size.
(4)
where T is the current value of the temperature gradient on the skin in polar coordinates, and T0 is the maximum value (at the pole of the corresponding isotherms).
Due to the fact that RO increases its size without changing the Z-coordinate, the magnitude of the positive gradient decreases due to the deteriorating thermal conductivity of the tissue in the CrT with 0.451W/(m.grad) instead of 0.532 W/(m.grad) in "normal", t .e. changes for the worse by 15%.25 This effect can be interpreted as a deterioration in the role of heat supply from the bottom wall of the CrT while simultaneously shielding the heat flux from the heat normal cells by the growing section of the CrT. When the upper boundary of the CrT contacts the skin of the MG, the normal flow at the point of contact on its surface disappears, since a zero gradient temperature appears in the pole, and with further growth of the PO, due to cutaneous elasticity, the upper border of the tumor is crushed, and thereby creating a negative temperature gradient8 at the isotherm pole as shown in Figure 3.
This is clearly seen in the case of two consecutively recorded mammograms in the lower menu, which indicate the average temperature in the RT, indicating which of the mammary glands contains any PT (if any are), what its shape and gradient are in it. All data are surveyed in a table located in the mammogram (Figure 4) (Figure 5) as upper menu, where given all the data obtained during the survey, and, in particular, the dimensions of the region of the projection of the gradient on the surface of the skin. These data are numerically estimated on mammograms.
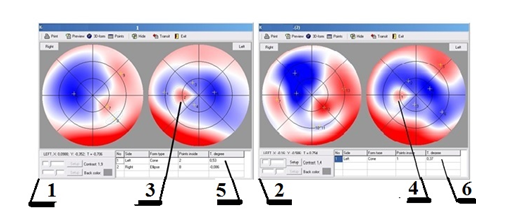
Figure 4 Two DOT mammograms 1 and 2, taken sequentially with an interval in 1 month, demonstrating the degradation of the tumor on the preclinical stage, dimensions of the region of the projection of the gradient (3 and 4), gradients (5 and 6).
As the tumor grows, the screening reveals the degradation of the heat flux maximum in terms of the intensity of the positive temperature gradient, as shown in Figure 3.
As can be seen from the above mammmograms and tables (Figure 5), the gradient and projection area data (4 and 3 in Figure 2 are 0.537 and 0.37°C, respectively) and 6.5 and 1.9% of the skin projection area MFs are well correlated and fit into the theory describing the development of breast cancer.26
The DOT method has several advantages with respect to CM. This is clearly seen in the example of the US standard recommended for examination of mammary glands, which is time-consuming and costly, but, as practice has shown, does not inspire confidence in clients whose breast cancer can be aggressive and the treatment belated.27
DOT method:
The paper discusses topical results on early and absolutely safe diagnosis of breast cancer with the help of the domestic DOT apparatus. Thanks to the design of this device, it is possible to use artificial intelligence with the help of a set of thermal examination data for the patient's MF for the effective choice of the treatment strategy by selecting the optimal therapy at this stage of breast cancer development with the help of pre-clinical prophylaxis.
None.
None.

©2018 Klukin. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.