Advances in
eISSN: 2573-2862


Clinical Images Volume 3 Issue 5
Department of Pathology, Ataturk Hospital, Izmir, Turkey
Correspondence: Naushi Engin Aydin, Department of Pathology, Ataturk Hospital Karabaglar, Izmir, Turkey- 35000 , Tel 90(546)6157058
Received: September 19, 2017 | Published: December 12, 2018
Citation: Aydin NE. External ear canal mass of long duration in an adult patient. Adv Cytol Pathol. 2018;3(5):122-124. DOI: 10.15406/acp.2018.03.00067
Syringocystadenoma papilliferum (SCAP) is a rare benign tumor of apocrine gland origin that usually occurs on the scalp and face area. Modified apocrine (ceruminous) glands located at the outer part of the external auditory canal (EAC) may be the origin of SCAP and result in a diagnostic challenge. An adult female patient with a long history of external auditory canal obstruction was diagnosed after an excisional biopsy of presumptive diagnosis inflammatory polyp. Immunohistochemical properties of the lesion was evaluated and SCAP was diagnosed histopathologically.
Keywords: syringocystadenoma papilliferum, external auditory canal, gross cystic disease, smooth muscle, ceruminous glands
SCAP, syringocystadenoma papilliferum; EAC, external auditory canal; GCDFP-15, gross cystic disease fluid protein-15; SMA, smooth muscle actin; CG, ceruminous glands
A woman in her 40s presented with a complaint of “unraveling external ear obstruction” of several years duration in the right external ear canal (EAC). Several attempts over the past years with local medications were made with out Complete recovery. There was no history of a biopsy and histopathologic examination. There was no hearing loss. She did not have neither history of general organ system problems nor tragal or mastoid tenderness in both ears. Right ear examination showed a well-circumscribed soft mass lesion in the bony part of the ear canal. It was not tender to touch, and the probe easily passed around the swelling.
Aspiration was attempted, with no fluid coming out. A presumptive diagnosis of a benign pathologic process such as inflammatory polyp was made and an excision biopsy of the lesion was undertaken under local anesthesia. The sample received was a nodular grey tissue measuring 0.8×0.6×0.3 cm. Microscopic sections from the tissue showed remnants of squamous epithelium and multiple invaginations and papillomatous proliferations of cuboidal, cylindrical epithelial cells (Figure 1).

Figure 1Exophytic epithelial proliferation showing papillary projections, invaginations, along with discernible squamous epithelial islands (Hematoxylin and eosin x 100).
There were small cystic spaces along with stroma showing inflammatory infiltrate rich in lymphocytes and plasma cells. The invaginations and cystic spaces were lined by either squamous epithelium near the surface or double-layered sweat gland epithelium with apocrine differentiation and decapitation secretion (Figure 2).
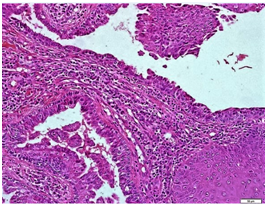
Figure 2 Squamous epidermal cell islands and cuboidal epithelial cells forming a double layer with lymphoplasmacytic inflammatory cells in the stroma, (Hematoxylin and eosin x 400).
Immunohistochemically CK5/6 was positive in the squamoid and some cuboidal/cylindrical cells in transitional areas (Figure 3). P63 was positive again in the squamous epithelial basal layers but not in the other components of the proliferation (Figure 4).
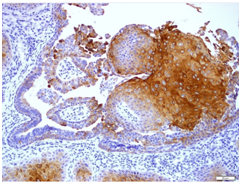
Figure 3 CK5/6 positivity in the squamoid and some cuboidal/cylindrical cells in transitional areas (DAB chromogene x200).
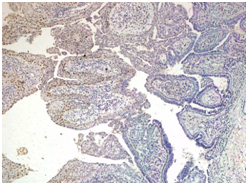
Figure 4 p63 positivity in the squamous epithelial basal layers but not in the other components (DAB Chromogene x100).
Gross cystic disease fluid protein-15 (GCDFP-15) revealed a prominent reaction at the near by ceruminous gland but was negative in the tumor cells (Figure 5). Smooth muscle actin (SMA) was positive at the basal layer of the invaginations and projections (Figure 6). Ki-67 proliferation index was only seen in the basal layers of the squamous type epithelium but not in cells of the papillary and invaginated structures (Figure 7).

Figure 5 GCDFP-15 showing a prominent reaction at the nearby ceruminous gland but was negative in the tumor cells (DAB chromogene x100).
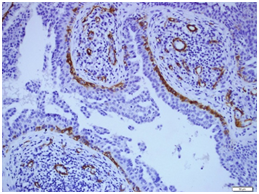
Figure 6 SMA was positive at the basal layer of the invaginations and projections (DAB chromogene x200).
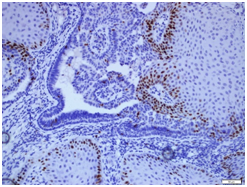
Figure 7 Ki-67 proliferation index seen in the basal layers of the squamous type epithelium but not in cells of the papillary and invaginated structures (DAB chromogene x200).
The histopathologic findings pointed to an unequivocal diagnosis of benign skin adnexal tumor, i.e.; syringocystadenoma papilliferium (SCAP) in the EAC. Modified apocrine glands i.e., ceruminous glands (CG) are located in the outer part of the EAC skin and CG benign tumors have been characterized as well-differentiated localized masses neoplasms that are occasionally cystic.1–3 The benign neoplastic growths of ceruminal neoplasms are, ceruminal gland adenoma (ceruminoma), pleomorphic adenoma and SCAP.
The microscopic structure of the lesion with papillary projections and invaginations lined with cuboidal and cylindrical cells with the luminal cells showing decapitation secretion are features of SCAP. SCAP has a well known association with a preexisting nevus sebaceous but there was no evidence of a nevus in this case. Mass lesions in the external auditory canal are difficult to diagnose based on clinical and radiological data. Histopathology usually represents the main diagnostic tool in these cases.
SCAP, despite its rarity, should be kept in mind in the differential diagnosis of mass lesions in the EAC.4,5 SCAP is an uncommon lesion representing approximately 5% of all tumors of the EAC canal and the auricle.1,2 Serious diagnostic difficulties may be encountered because of varied clinical and histological manifestations. Histologically, endophytic invaginations of epithelium extend from the epithelial surface into the dermis. Typically squamous epithelium is present at the surface of the invaginations, and is contiguous with a double layer of cuboidal and columnar epithelium in the deeper portions of the lesion. Within the dermis, broad villous projections protrude into cystic spaces.
Columnar epithelium is present toward the lumen of the spaces, and simple cuboidal epithelium can be seen at the periphery. Decapitation secretion of luminal cells is a frequent finding. The basal cell layer is positive for SMA but GCDFP-15 a marker for apocrine differentiation shows in consistent resuts2,5,7 and may be negative as in this case. Plasma cells are consistently numerous with in the stroma, and are a highly reproducible finding in the stroma of SCAP.
SCAP presenting as a soft tissue mass that persist in the EAC should be differentiated from other benign neoplasms, such as papilloma, ceruminous gland tumors besides malignancies such as squamous cell carcinomas, and even inflammatory reactive epithelial proliferations1–5,7 and in addition malignant but rare variant of SCAP should be kept in mind.6,7 SCAP may be a real diagnostic challenge for a pathologist. Squamous epithelium covering the tumor is a non specific structure that can also cover cysts, fistulas, and other tumors. The patient showed complete healing and there was no recurrence after a one year follow-up.
There were no funding sources for the study.
The author declares no conflict of interest.

©2018 Aydin. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.