Advances in
eISSN: 2573-2862


Case Report Volume 3 Issue 5
Department of Pathology and Orthopaedics Surgery, Aligarh Muslim University, India
Correspondence: Kafil Akhtar, Department of Pathology, Jawaharlal Nehru Medical College, Aligarh Muslim University, India
Received: August 26, 2018 | Published: November 19, 2018
Citation: Haiyat S, Alam S, Akhtar K, et al. Disseminated crytptococcosis presenting as fracture of clavicle and humerus. Adv Cytol Pathol. 2018;3(5):115-117. DOI: 10.15406/acp.2018.03.00065
A 26year old male presented to the orthopaedics out-patients clinic with a 5months history of progressive pain and swelling in the left shoulder, without fever, night sweats, cough, weight loss, headache and altered sensorium with no meningeal signs. He had no medical history of diabetes, chronic renal disease, tuberculosis, alcoholism, leukaemia, lymphoma, AIDS, Hodgkin’s disease, corticosteroid intake or any organ transplantation. A preoperative blood count, liver and renal function, blood sugar levels, and tumor markers were all normal. Serological tests were negative for HIV and Hepatitis. X ray revealed multiple lytic lesion over the clavicle and proximal humerus with fracture. On MRI scan, multiple ring enhancing lesions depicting solid cryptococcoma were observed in the brain parenchyma. Biopsy from the bone and culture revealed cryptococcal infection. He was treated with surgical debridement combined with antifungal therapy for 8weeks. After 6months of follow up, the fracture healed well with no evidence of recurrence.
Keywords: cryptococcal meningitis, fungal infection, fracture, histopathology
Cryptococcus neoformans is an encapsulated yeast like fungus that is widely distributed in nature. It is usually found in large numbers in soil contaminated by pigeon roosts.1 This infection is most commonly seen in people who are immunocompromised, such as those with HIV infection, leukaemia, lymphoma, Hodgkin’s disease, as well as in patients on high doses of corticosteroid medications and cancer chemotherapy.2 However immunocompetent patients are rarely afflicted with this disease, with incidence estimated to be 0.2per million per year.3
Infection results from inhalation of aerosolized spores, which germinates in lung and disseminates to the central nervous system causing meningoencephalitis.4 Skeletal involvement is very uncommon and is documented in only about 5%-10% of patients with disseminated cryptococcosis.5,6 Most of the skeletal cryptococcosis are osteolytic in nature arises secondary to hematogenous spread from a primary infection. The radiological features of osseous cryptococcosis are non-specific and the findings simulates to those of osseous tuberculosis and other neoplastic lesions.7‒9 There have been very few cases reported of skeletal cryptococcosis and to our knowledge and extensive research the involvement of humerus and clavicle by the latter is not documented in literature. We are here presenting a unique case of cryptococcal meningitis in a young immunocompetent man who presented with pathologic fracture of the clavicle and proximal humerus.
A 26year old Indian male presented to the orthopaedics out-patients clinic with a 5months history of progressive pain and swelling in the left shoulder, without fever, night sweats, cough, weight loss, headache and altered sensorium. Physical examination showed no meningeal signs. He had no medical history of diabetes, chronic renal disease, tuberculosis, alcoholism, leukaemia, lymphoma, AIDS, Hodgkin’s disease, corticosteroid intake or any organ transplantation. Laboratory workup showed mild increase in erythrocyte sedimentation rate of 28mm/hr with normal C reactive protein of 4mg/l. A preoperative blood count, liver and renal function, blood sugar levels, and tumor markers were all normal. Serological tests were negative for HIV and Hepatitis.
X ray of the left upper arm showed multiple lytic lesion over the clavicle with the fracture of the surgical neck of humerus showing marked displacement (Figure 1). Surgical debridement was done and the material was sent for histopathology. Haematoxylin & Eosin stained section revealed numerous round to oval encapsulated yeast like organisms mostly in singles and occasionally as budding yeasts. Per-iodic acid schiff stain showed variable sized encapsulated yeast cells with prominent capsule (Figure 2). The Grocott’s methenamine silver (GMS) stained tissue section also showed typical encapsulated yeast cells morphologically consistent with Cryptococcus.
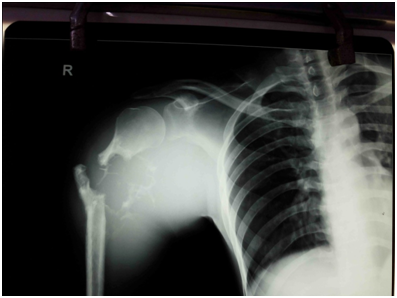
Figure 1 X- ray of the left upper arm showed multiple lytic lesion over the clavicle with the fracture of the surgical neck of humerus showing marked displacement.
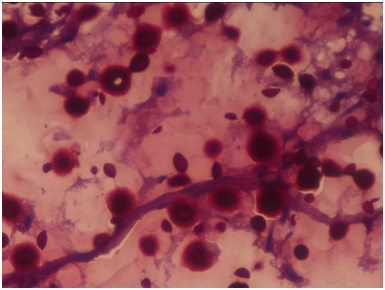
Figure 2 Tissue section stained by PAS stain shows variable sized numerous encapsulated yeast cells with prominent capsule. PAS stainx 40X.
MRI scan was later performed with the suspicion of involvement of brain which highlighted multiple ring enhancing lesions depicting solid cryptococcoma in the brain parenchyma (Figure 3). Microbiological culture on Sabouraud’s dextrose agar showed dark cream coloured smooth moist mucoid colonies positive for Cryptococcus (Figure 4). India ink staining also highlighted the budding yeast cells of C. neoformans surrounded by a characteristic wide gelatinous capsule (Figure 5). All the above investigations confirmed the diagnosis of cryptococcal meningitis. The patient was given intravenous amphotericin B (0.8mg/kg/day) and 5-fluorocytosine (1mg/kg/day) for 8weeks. After 6months of follow up, the fracture healed well with partial resolution of the lytic lesion and no signs of disease progression.
Cryptococcal meningitis is a potential fatal infection caused by the fungus Cryptococcus neoformans. C. neoformans is a spherical yeast like fungus measuring 4-6micron in diameter surrounded by a polysaccharide capsule.10 This infection is common in adults, affecting males more than females, with a predominance of 55%- 75%.1
Infection results from inhalation of aerosolized basidiospores. The most common clinical form of the disease is meningitis, which develops by way of hematogenous dissemination from the lung to the central nervous system (CNS).4,5 The onset of cryptococcal meningitis is insidious and simulates other forms of chronic meningitis such as tuberculosis. Dull occipital headache, fever, drowsiness, and alterations of consciousness or behaviour may be presenting features. Visual impairment may also develop. On examination, stiffness of the neck is often found and focal neurologic deficits may be elicited. Progression is slow in most cases, but the process is ultimately fatal if the patient is not treated.
The incidence of the osseous involvement is low, manifested in only 5%-10% of patients with disseminated cryptococcosis.5,6 The common sites affected are the lumbar spine, pelvis, ribs, and skull in cases of isolated bone cryptococcosis.11‒13 Usually these lesions are lytic on radiograph and should be kept under the differential diagnosis of lytic lesion of bone. The symptoms of skeletal cryptococcosis are atypical, and it is difficult to diagnose with a simple physical examination. Biopsy with demonstration of the infectious organism is the gold standard for diagnosis. Approximately only 30.4% of patients who have radiographic evidence of infection will have positive blood cultures.13‒15 A combination of anti-fungal drugs mainly amphotericin B, fluconazole, and flucytosine are given for a course of six weeks.15‒17
There are very few cases of osseous cryptococossis mentioned in the literature. The unique presentation as multiple fractures at a rare site and the immuno competence of the patient makes this case very unique and interesting.
None.
The authors declare that they have no Conflict of interest.

©2018 Haiyat, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.