Comparison of the postoperative analgesic effects of intrathecal Clonidine and Fentanyl as adjuvant: mata analysis of randomized control trials
1Department of Anesthesia, Bahir Dar University, Ethiopia
2Department of Anesthesia, University of Gondar, Ethiopia 3Department of Microbiology, University of Gondar, Ethiopia Received: April 04, 2019 | Published: April 30, 2019
Correspondence: Fantahun Tarekegn, Department of Anesthesia, Bahir Dar University, Ethiopia, Tel +251966856865 Citation:
Tarekegn F, Hailekiros A, Eshetie S. Comparison of the postoperative analgesic effects of intrathecal Clonidine and Fentanyl as adjuvant: mata analysis of randomized control trials. J of Anes & Cri Open Access. 2019;11(2):52‒58. DOI:
10.15406/jaccoa.2019.11.00411
AbstractBackground: Intrathecal clonidine and fentanyl added to bupivacaine prolongs the postoperative analgesic effects for below umbilicus surgery. However, the overall effect of clonidine and fentanyl mixed with spinal anesthesia is not harmonized. Therefore, the aim of this Meta - analysis was to assess the post operative analgesic effects of intrathecal clonidine and fentanyl for different randomized control trials of study. Methods: Pubmed, Cochrane Review, EMBASE, and Google Scholar were searched and a total of four studies have been selected for Meta – Analysis. Three authors engaged independently to extract data on the efficacy of intrathecal clonidine and fentanyl for lower abdomen and limb surgeries. The statistical analysis was accomplished by RevMan (version 5.3) software. The overall efficacy of intrathecal clonidine and fentanyl were pooled by Forrest plot, table, and figure with 95% confidence interval. Results: A total of 310 patients from four studies were included in this Mata analysis. The results showed that intrathecal clonidine resulted statistically significant longer duration of analgesia compared to fentanyl with mean difference of [83.57(95 % CI, 29.33 to 137.82), I2=97%, P<0.00001] minutes. Furthermore, mean difference of clonidine sensory block [26.27(95% CI, 4.13 to 48.42), I2=97%, P<0.00001] and motor block [26.06(95%CI, -0.23 to 52.34), I2 =98%, P<0.00001] minutes respectively were significant compared to fentanyl. Conclusion: Intrathecal clonidine as adjuvant to bupivacaine gave the prolonged postoperative analgesia in comparison to intrathecal fentanyl. So it is recommended to use clonidine as intrathecal adjuvant when we consider the extended postoperative analgesia. Keywords: intrathecal, clonidine, fentanyl, postoperative analgesia, bupivacaine AbbreviationsCI, Confidence Interval; IV, Inverse Variance, MD: mean difference, SD, standard deviation BackgroundSpinal anesthesia is the routine done procedure with bupivacaine for below umbilicus and lower limb Surgeries. This type of regional anesthesia is ensuring intraoperative and early postoperative period pain management, despite its restricted duration of action.1 In turn, to increase duration of analgesia and quality of blockage, adjuvant of intrathecal clonidine and opioids are appropriate.2 Different studies have been found that intrathecal midazolam, neostigmine, opioids and clonidine put together the prolongation of subarachnoid block and reduction of postoperative analgesic consumption.3−7 Specifically, addition of low doses of clonidine and fentanyl in intrathecal could be associated with lesser incidence of adverse effects.8 However, intrathecal opioids with bupivacaine connected with side effects of nausea, vomiting, pruritus, respiratory depression and urinary retention in favor of clonidine which has not this property.9 Amongst the opioids, fentanyl could be the choice of adjuvant because of its potency, rapid onset and short duration of action with lesser incidence of respiratory depression.8,10 Even though rising number of published trials with small number of patients paying attention on post operative analgesic effects to intrathecal clonidine and fentanyl, full up to date evidence in larger population is lucking so far. Therefore, it was the aim of this Meta analysis performed to confirm their conclusion using at larger sample size. MethodsStudy selection A literature search was conducted in Pubmed, Cochrane review, EMBASE and Google scholar data bases and articles which are relevant to our study were identified. The search was performed by three authors (FH, AH, SE) independently with asking the key words of intrathecal, clonidine, fentanyl and postoperative analgesia. In the middle of citation extracted, abstracts were reviewed to recoup the clinical studies of randomized control trials on intrathecal adjuvant of clonidine and fentanyl. Articles that were related, by title and abstract were right to used in full text to determine those that provided sufficient information to be included in our Meta-analysis. Inclusion and exclusion criteria The trials included in our Meta analysis: patients undergoing spinal anesthesia were assigned to at least two groups, including Clonidine alone as an adjuvant to local anesthetics and Fentanyl alone as an adjuvant to local anesthetics. So, all randomized control trial studies investigating the efficacy of intrathecal clonidine (50µg) compared with intrathecal fentanyl (25 µg) for patients under went to lower abdomen and extremity surgery. Outcome of interest The primary outcome of interest was duration of Analgesia. The secondary outcomes of interest were duration of sensory and motor blockage. Data extraction Data from qualified studies were extracted independently by authors and summarized into a spreadsheet. Discrepancies were resolved by agreement. For each of the included studies, the following information was extracted; First author’s name, year of the study, numbers of patients/study participants, total volume for spinal anesthesia, and types of surgery (Table 1).
Table 1 Characteristic of the included studies Notes *values are mean±standard deviation. Abbreviation: C, Clonidine; F, Fentanyl; Bup, Bupivacaine
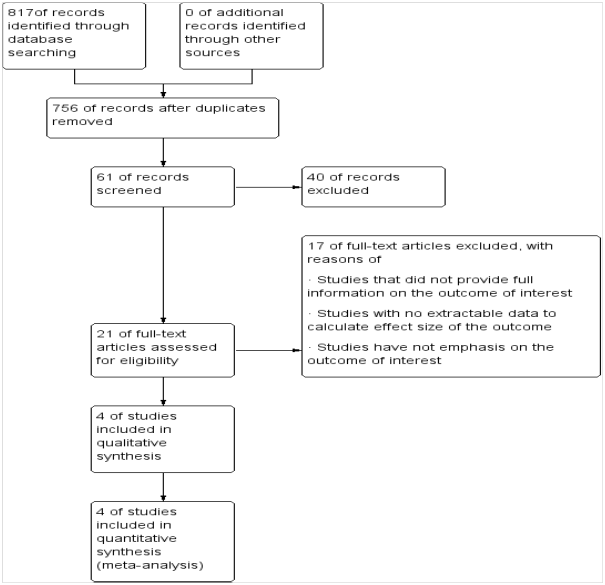
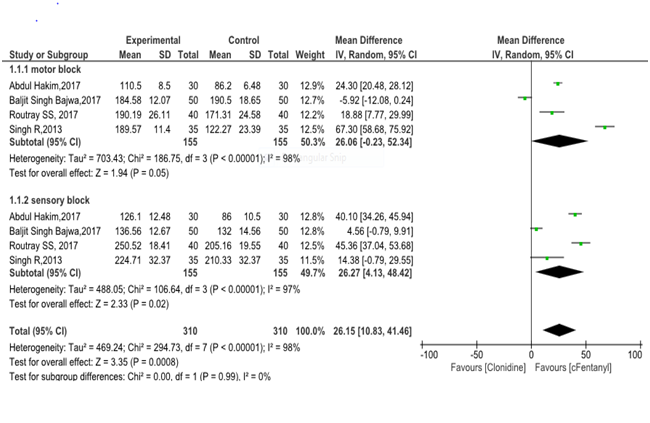
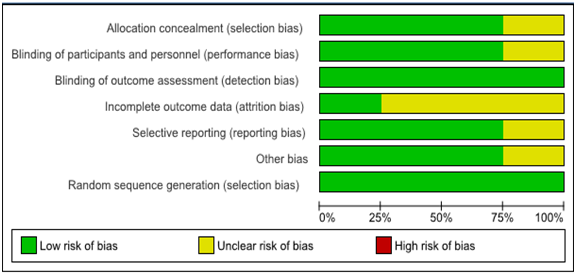
Three authors (FT, AH, SE) examine the full-text articles and they independently decided whether the retrieved trials met the inclusion criteria or not. The Two authors (FT, AH) carried out the data extraction using special standardized forms developed for the Meta analysis. These included titles, contact information of the authors, type of surgery, and types of intrathecal adjuvant. The outcome data were entered into RevMan 5.3 provided by the Cochrane Collaboration for further statistical analysis. Quality control Two authors (FT, AH) independently read and evaluated the methodological validity of all eligible studies using a set of prearranged criteria of research design, quality of paper, and engaged methods for intrathecal clonidine and fentanyl. Any discrepancies were resolved through joint discussion, if necessary a third researcher assisted in the decision. Data analysis A randomized effect model was used to determine the outcomes of analgesic effects of clonidine and fentanyl adjuvant with 95% confident interval. We evaluated the heterogeneity of study results with the use of I2 test and random effect (RE) model. Significant heterogeneity was considered P<0.10 and I2>50%.12,13 The overall effect size of time of first analgesic request for Intrathecal clonidine versus fentanyl was pooled by the forest plot with 95% CI. Statistical analysis was performed by the use of Cochrane review manager (RevMan 5.3). Results We have found 817abstracts through electronic data base search. Among this studies756 were ignored after reviewing their titles and reached to 61 screened articles. Then 40 articles were excluded due to the abstracts or full text information did not related to the topic interest. 17 were excluded from the 21 assessed eligible studies with some reasons of exclusions criteria. Eventually, four articles fulfilled our eligibility criteria and were subjected to Meta analysis (Figure 1). Selected articles were published from 2013 to 2017 (Table 2). As shown from Figure 2 a mean difference (MD)=[83.57(95 % CI, 29.33 to 137.82), I2=97%, P<0.00001] minutes. The highest and lowest mean difference of effect sizes were MD=175.98 and 10.60 minutes respectively. Furthermore, the selected four articles in Fig 3 put that the pooled mean difference of duration of sensory and motor block were MD=(26.27 and 26.06, I2=98% , p<0.00001 ) minutes respectively at postoperative period. In Fig 4 also represented the degree of risk of bias for integrated studies. 
Figure 2 Forest plot of the pooled effect size of the intrathecal Clonidine versus Fentanyl for Postoperative analgesia underwent lower Abdomen and lower Limb Surgeries.
Table 2 Summary of results from the indivial studies Notes *values are mean±standard deviation. Abbreviation: C, Clonidine; F, Fentanyl DiscussionSpinal anesthesia is a type of neuraxial regional anesthesia which covers for lower limb and lower abdominal surgeries. However, plain local anesthetics associated with cardiac and neurological toxicities.14,15 For reduction of this, spinal anesthesia agents were mixed with other drugs, to decrease the dose requirement and potentiation of the duration of regional anesthesia.11 This Meta analysis of randomized control trials showed that 50µg intrathecal clonidine as an adjuvant provided the prolonged postoperative analgesia compared with 25µg intrathecal fentanyl as a mean difference (MD) of [83.57(95%CI, 29.33 to 137.82), I2=97%, P<0.00001] minutes. Different studies have been found that both clonidine and fentanyl added to spinal block with bupivacaine are effective for the persistence of postoperative analgesic time.16,17 It was also supported by other different studies which gave the evidence of 50µg clonidine to intrathecal bupivacaine made the lengthening of analgesic duration in comparison to 25µg fentanyl with bupivacaine.18−20 In regarding to secondary outcomes of interest Mata analysis study, the sensory and motor duration of block is significantly prolonged in intrathecal clonidine group compared to fentanyl. This was consistent with many different studies.19−22 However, there was not considerable inter sub group differences of block duration between the motor and sensory. The means of clonidine related potentiation of spinal sensory block is reported to be reliant on presynaptic (decrease transmission) and postsynaptic (hyper polarization) action. It activates the α2 receptors with blocking of Aδ and C nerve fibers at substantia gelatinosa of spinal cord to generate analgesia.23,24 Fentanyl is the preferred opioid drug for regional anesthesia with action on µ1 and µ2 receptor agonist. It is highly potent drug due to high lipid solubility25,26 despite some related complications of nausea, vomiting, and pruritus.27 According to some study, even at higher dose of clonidine (450µg) only in intrathecal, didn’t result muscle weakness and motor block,28 but combination to spinal bupivacaine caused significant enhancement of the strength and duration of motor block.29,30 Tilkar et al.31 study compared clonidine and fentanyl added to intrathecal bupivacaine and reached as conclusion of clonidine was more helpful than fentanyl in pain-relieving properties.31 Even though different studies have been used intrathecal clonidine from dose of 15µg to150µg, the 50µg intrathecal clonidine was provided the extended postoperative analgesia with minimal side effects compared to fentanyl.32−34 There are a number of limitations to our Meta analysis. It was possible to miss some studies which satisfied the inclusion criteria, and number of studies to be excluded as the full text was unavailable. In addition, there was significant heterogeneity to duration of analgesia, duration of sensory block and duration of motor block with considering different doses of bupivacaine drug and types of surgery (Figure 3) (Figure 4). ConclusionAddition of 50µg clonidine to intrathecal bupivacaine, put forward the longer duration of postoperative analgesia than 25µg of fentanyl. So, it is recommended to use clonidine when we consider the extended duration of postoperative analgesia. AcknowledgementsWe would like to thank Mr. Awoke in department of Microbiology, Bahir Dar University for helping with suggestion on meta-analysis and systematic review. Availability of data and materialsNo additional data are required; all information is clearly presented in the main manuscript. FundingWe have not any source of funding. Competing interestsThe authors declare that they have no competing interests. Authors’ contributionsFT: Conception of research protocol, study design, literature review, data collection, data extraction, data analysis and interpretation, and drafting manuscript. Consent for publicationNot applicable. Ethics approval and consent to participate
References
 © 2019 Tarekegn et al. This is an open access article distributed under the terms of the Creative Commons Attribution License
, which
permits unrestricted use, distribution, and build upon your work non-commercially.
© 2019 Tarekegn et al. This is an open access article distributed under the terms of the Creative Commons Attribution License
, which
permits unrestricted use, distribution, and build upon your work non-commercially.
|