Advances in
eISSN: 2377-4290


Case Report Volume 4 Issue 2
Department of Ophthalmology and Visual Science, Yale University, School of Medicine, USA
Correspondence: Brian M DeBroff, Associate Clinical Professor, Yale University School of Medicine, Ophthalmology Surgical Services, Department of Veterans Affairs, West Haven 950 Campbell Avenue, West Haven CT 06516, USA, Tel (203) 785-1755
Received: March 08, 2016 | Published: March 26, 2016
Citation: DeBroff BM, Kalyam K. Lens fragment removal from the anterior chamber using cannula aspiration. Adv Ophthalmol Vis Syst. 2016;4(2):52-54. DOI: 10.15406/aovs.2016.04.00104
Retained nuclear and cortical material is increasing after phacoemulsification cataract surgery. Most surgeons use irrigation/aspiration hand tips to remove such particles when they are identified. We offer an alternative method using a cannula to improve visualization and decrease turbulent infusions.
Keywords: lens fragments, retained nuclear material, retained cortical material, anterior chamber residual material, post-operative complications after phacoemulsification cataract surgery, cannula aspiration
Retained lenticular material in the anterior chamber after phacoemulsification cataract surgery is increasing and can lead to inflammation, increased intraocular pressure and corneal edema/decompensation. If these fragments can be identified before concluding the surgical procedure, these complications can be prevented. We describe a case in which a lenticular fragment is identified and describe a novel technique of using a cannula to remove the piece rather than the typical re-insertion of the irrigation/aspiration handpiece which can actually create turbulent flow and lead to loss of the fragment under the iris or in the ciliary sulcus.
An 86 year old male underwent phacoemulsification cataract extraction with posterior chamber intraocular lens implantation in the left eye. His pre-operative refraction OS was +1.25-1.25 x 95 and his axial length OS was 23.74 and average K’s OS were 42.46. A temporal clear corneal incision was performed with a 2.2 mm keratome and a 1.0 mm side port incision was performed inferiorly. The nucleus was removed in a stop and chop technique and cortex aspirated with the irrigation/aspiration handpiece. There were no complications during the procedure. Upon hydration of the side port incision, a small lenticular particle was observed anterior to the IOL in the anterior chamber (Figure 1).
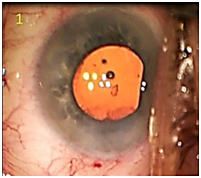
Figure 1 Microscopic view of lens fragment anterior to posterior chamber intraocular lens in the capsular bag.
A 23 gauge-cannula on a 3ml syringe filled with balanced saline was placed through the side port incision (Figure 2). Minimal irrigation was used to maintain the anterior chamber depth. The cannula tip was advanced toward the lenticular fragment and secured to the tip by gentle aspiration (Figure 3). Once the fragment was secured, slightly more aggressive irrigation was used to draw the material into the cannula (Figure 4). No flattening or fluctuation of the depth of the anterior chamber was observed. The cannula was then removed from the eye and the anterior chamber was observed to be free of any residual material (Figure 5). The patient’s post-operative course was unremarkable with normal intraocular pressure, clear cornea, and quiet anterior chamber by 2 weeks after surgery with all drops tapered off by 3 weeks post-operatively with best corrected vision of 20/25 OS. The fundus showed no abnormalities other than retinal pigment epithelium changes that were present prior to the cataract surgery.
Retained nuclear or cortical lens chips in the anterior chamber after phacoemulsification cataract surgery are occurring more frequently1–8 especially with phacoemulsification tips using torsional or transitional movement.9 Dada et al.,10 discovered nuclear fragments in 65 of 1000 eyes just prior to ophthalmic viscosurgical device removal. In addition pretreatment of the nucleus creating multiple grid-like channels using a femtosecond laser can lead to small loose lens fragments that can escape aspiration by the phacoemulsification tip. Retained lens fragments have been reported to more likely occur in high myopes and steep keratometry, patients with small pupils, floppy iris, highly retentive viscoelastic, use of iris hooks, and hard nuclei.1,8,9,11 Hui et al.,1 found that axial length longer than 24.0 mm or keratometry greater than 45.00 diopters resulted in deeper anterior chambers and a higher incidence of lenticular fragments. It is common for small lenticular or cortical material to avoid visualization and detection in the anterior chamber angle or under the iris. Oliveira described cases in which a bulge in the iris led to discovery of retained nuclear fragments.12 Retained nuclear fragments have been described initially presenting many years after cataract surgery and only may be visualized using gonioscopy.13,14
In addition, small lenticular fragments can become trapped in the main incision or side port incision and later become displaced into the anterior chamber.2,3,15 Surgeons should always inspect the incision sites to identify any residual cortical or lenticular material.6,9 At times these fragments only become apparent once the surgery is completed or wounds are sealed with hydration. Retained nuclear fragments in the anterior chamber can lead to persistent iritis, corneal edema, corneal pannus, and corneal decompensation which have necessitated penetrating keratoplasty 1,9,13, and increased IOP or glaucoma.1–4,8,14 In most cases, the symptoms tend to resolve with surgical removal of the lens fragment.1,14 Osher states that the best prevention is vigilance, identification of the chip, and prompt removal.6
Use of a cannula to remove subincisional cortex has been described as a method that provides superior visualization, less irrigation, more efficiency, and less swirling of the contents of the anterior chamber which is associated with the irrigation/aspiration method.16 Also mashing a fragment into the I/A handpiece can lead to smaller pieces breaking off and being retained due to lack of visualization.14 We now describe a case using the technique of employing a cannula to remove a small nuclear fragment from the anterior chamber. Similar to its use in the removal of cortical material, use of a cannula for removal of a lens chip provides excellent visualization.
In addition, using the cannula prevents the need for re-entering the eye with the irrigation/aspiration hand piece. The I/A handpiece can often lead to infusional currents and turbulence that may drive the material out of view and lead to loss of the chip under the iris or deep in the ciliary sulcus and cause unsuccessful attempts at removal.1,8 By carefully controlling small degrees of direct aspiration using a cannula, the fragment can be safely and quickly removed with little trauma and avoidance of future complications of retained lenticular material. If one encounters an excessively large fragment or a particularly dense brunescent fragment, a larger cannula or phacoemulsification probe may be necessary, however, most small fragments should be successfully removed using a cannula with manual aspiration.
None.
None.
The author declares there are no conflicts of interest.