eISSN: 2377-4304


Case Report Volume 7 Issue 2
Department of Obstetrics and Gynecology, Centro Hospitalar Medio Ave, Portugal
Correspondence: Amelia Maria de Almeida, Department of Obstetrics and Gynecology, Centro Hospitalar Tmega e Sousa, Avenida Padre Am?rico-Guilhufe, Penafiel, Porto 4560-007, Portugal
Received: October 27, 2016 | Published: May 29, 2017
Citation: Almeida AM, Marinho C, Figueiredo O, Enes P, Oliveira C (2017) Oblique Muscle Hematoma: A Gynecologic Surgery Complication?. Obstet Gynecol Int J 7(2): 00242. DOI: 10.15406/ogij.2017.07.00242
Gynecologic surgery complications are varied and their frequency depends of surgery type and the patient´s comorbidities. Abdominal wall hematomas are uncommon cause of abdominal pain and it´s misdiagnosed. Most of abdominal wall hematomas are localized in rectus sheath and an oblique hematoma is a very rare condition with a few publications in literature.
The authors report an oblique muscle hematoma in a patient underwent an abdominal hysterectomy without complications. In sixth day after surgery, she was admitted with acute right low back pain and fever. Abdominal computerized tomography and ultrasound showed a hematoma on the right oblique muscle. After diagnosed of oblique hematoma patient was treated conservatively.
An oblique hematoma muscle should be considered in differential diagnosis of lateral abdominal or low back pain (if presenting with echymosis). With this case the authors highlight a rare pathology that may be more frequent in the future due the increased number of anti-coagulated patients.
Gynecologic surgery complications may be classified as anesthesia related, hemorrhagic, infectious, urinary, gastrointestinal, vascular and nervous. The complication rate varies according to the type of surgery and patient´s comorbidities.1 Abdominal muscle hematomas are rare, but they may be a complication associated to any abdominal surgery including gynecologic. Most abdominal wall hematomas occur in rectum sheath, and hematomas within the oblique muscle are unusual. Women over 50 years old present hematomas more often than men, probably due to their muscular fragility.2 In this article, the authors present a clinical case of a hematoma of the oblique muscle after a gynecologic surgery and its further complications.
A Caucasian woman, with 44 years old with a previous history of essential hypertension and no previous abdominal surgeries. The preoperative tests made one month before the surgery demonstrated a hemoglobin level of 13.5g/dl. She did venous thromboembolism prophylaxis with 40 mg subcutaneous enoxaparine initiated 12 hours before surgery and during the entire hospital stay. The patient underwent an abdominal hysterectomy due to menorrhagia related to uterine leiomyoma. The surgery was uneventful. On the third day, a lower urinary tract infection was diagnosed and treated with empiric antibiotic therapy (amoxicillin + clavulanic acid). The patient discharged hospital on the fourth day after surgery with adequate postoperative evolution.
On the sixth day after surgery, the patient was admitted to the emergency room (ER) with right low back pain with anterior irradiation and hyperthermia. At ER the patient presented with axillary temperature of 38.2oC, hemodynamic stability, and slightly colorless but hydrated mucous. Abdomen was soft but very painful at palpation on the right flank without peritoneal signs. An ecchymosis with 5 cm was observed on the right low back area. The surgical scar was reddish, without any inflammatory signs. The gynecologic exam was normal. A renal ultrasound was performed and it only showed a thickening of the right lateral abdominal wall. A abdominal computerized tomography (CT) scan was performed to clarify the thickening, and it revealed thickening of the right oblique muscle with 95x35mm, suggesting oblique muscle hematoma, without any signs of active hemorrhage (Figure 1). Blood count revealed hemoglobin 9.6g/dl, leucocytes 11.900 with 87% neutrophils, CRP 338, and normal renal function. The microbiologic urine test made on the 3rd day after surgery isolated an E. Coli resistant to amoxicillin and clavulanic acid. Reexamination of the patient revealed a subcutaneous hardening at the site of the ecchymosis that was extremely painful at palpation, she denyabdominal trauma.
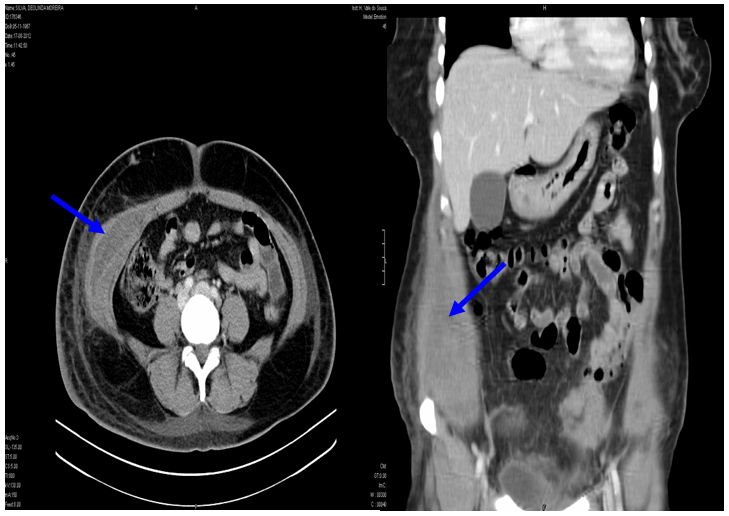
Figure 1 Computerized tomography shows a oblique of right oblique muscle and asymmetric thickening of the oblique muscles (blues arrows).
The patient was admitted to our department for expectant management, with recommendation to rest, and an application of ice packs on the hematoma site. She did oral analgesic, and antibiotic therapy was changed to piperacillin+tazobactam and clotrimazole. During the next 48 hours, the patient did not present fever, remained hemodynamically stable and the hematoma maintained the same dimensions. Further lab tests revealed hemoglobin 10g/dl, with stabilization of the inflammatory parameters. Control CT scan of the abdomen and pelvis on the 12th day after surgery showed an oblique hematoma with 55x45mm (Figure 2). The patient discharged the hospital on 20th. At follow-up appointment (3rd and 6th months after surgery), the patient was clinically well. Hemorrhagic dyscrasias were excluded, and the abdominal and soft tissues ultrasound didn´t reveal any anomalies.
Abdominal hematomas may result from the rupture of epigastric vessels, of the circumflex iliac artery, low back arteries, subcostal arteries or from the rupture of the abdominal rectus or oblique muscle fibers.3,4 Rectus and abdominal oblique muscle hematomas are difficult to diagnose because are rare and these presentations could resemble other pathologies. Abdominal pain, back lower pain, fever and ecchymosis are the most frequent symptoms and signs and may simulate acute abdomen or pyelonephritis.2 In a study conducted by Cherry et al.5 only 17% of the abdominal hematomas present ecchymoses.5 In our clinical case, diagnosis was made only after the appearance of the ecchymosis and pain, and when abdominal CT scan was performed. Our first diagnostic hypothesis, when patient presented in ER and before the complementary exams was acute pyelonephritis. We based this first diagnostic on several of the patient´s symptoms, such as unilateral back pain, fever, positive Murphy´s sign on the right side and urinary tract infection with isolation of E. Coli resistant to the antibiotic therapy given. After blood count and CT scan this hypothesis was excluded.
Traumatic or non traumatic aggressions, such as excessive muscle distention or contraction due to coughs, vomit or sneezing; fragility of the blood vessels or of the muscles caused by arterial hypertension, atherosclerosis, old age, obesity, pregnancy and previous surgeries; anticoagulant therapies; coagulation alterations and hemorrhagic dyscrasias may cause abdominal muscle hematomas.1,3 Cherry WB et al.5 conducted a review of 126 cases of abdominal rectus muscles hematomas, and observed that in 69% of the cases the most common cause was the use of anticoagulant therapy.5 In our clinical case, the patient was under prophylactic anticoagulant treatment and her coagulation tests were normal. Although anticoagulant therapy is pointed out as the main cause of abdominal wall hematomas, we did not find any study that associates the use of prophylactic doses of anticoagulants with abdominal wall hematomas.
Diagnosis of abdominal muscles hematomas is made based on the patient´s clinical history, physical exam, clinical tests and other complementary imaging exams. Ultrasound of the soft tissues and CT scan are indicated for the diagnosis of abdominal wall hematomas. Ultrasound is first choice when there is no suspected diagnosis or when a CT scan is not readily available.4
When there is suspected abdominal hematoma, active hemorrhage or need for better characterization of the hematoma, a CT scan is indicated in view of its more detailed features.6 Diagnosis or suspected diagnosis of oblique muscle hematoma is a fundamental step for it may avoid unnecessary surgeries (suspected acute abdomen), which can change our patient management. In our case, there was suspected hematoma only on the 5th day after surgery, when the patient was submitted to a renal ultrasound due to suspected acute pyelonephritis, which allowed us to recommend expectant treatment and adequate therapeutic measures.
The conservative treatment consists of rest, analgesic therapy, fluid therapy when necessary and, placing ice packs on the hematoma area. There is no consensus regarding the use of antibiotics: some authors advocate their use only if there are signs of infection, and not as prophylaxis.3
Surgical treatment or arterial embolization procedures are adopted only in cases of unsuccessful conservative treatments, i.e. when hemorrhage remains active.6 Mortality rate is low, but it can reach 4%.6 Our patient has urinary tract infection and fever, so we opted to maintain a larger spectrum antibiotic therapy.
The oblique muscle hematoma does not have any classification as does the rectus muscle hematoma, which is classified in 4 stages. Due to the rarity of oblique muscle hematomas, there are no studies in the literature that support the use of the same classification adopted for rectus muscles hematomas.7 We were not able to reach a conclusion about the pathophysiology of the hematoma or which vessel caused the hemorrhage. However, the patient did present some risk factors that may have triggered the hematoma: hypertension, abdominal surgery and anticoagulation therapy. Essential hypertension causes fragility of the blood vessels, which increases the formation of hematomas. The incision on abdominal wall may harm blood vessels and abdominal muscles, but it is very difficult to find a case in which a Pfannenstiel incision caused any lesion to the oblique muscle. Surgical retractors may have caused oblique muscle distention or a lesion on a vessel that communicates with the circumflex artery, causing hemorrhage.
There are very few cases of oblique muscle hematomas described in medical literature, and none of them are presented such as a complication of an abdominal surgery. In this article, the authors highlight this rare pathology that may become more frequent in the future with the increase of anticoagulant therapies and shouldn´t be forgotten in differential diagnostic of abdominal or lower back pain post abdominal surgery.
None.
None.

©2017 Almeida, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.