MOJ
eISSN: 2471-139X


Case Report Volume 4 Issue 4
1Department of Anatomy, Kampala International University, Uganda
2Department of Radiology, Crystal Specialist Hospital, Nigeria
3Department of Anatomy, University of Lagos, Nigeria
4Department of Physiology, Kampala International University, Uganda
5Department of Physiology, University of Ilorin, Nigeria
Correspondence: Afodun Adam Moyosore, Department of Anatomy, Faculty of Biomedical Science, Kampala International University, Uganda, Department of Radiology, Ultrasound and Doppler Unit, Crystal Specialist Hospital, Akowonjo-Dopemu, Lagos, Nigeria, Tel 2348077295769
Received: September 07, 2017 | Published: November 13, 2017
Citation: Moyosore AA, Adeola BA, Daniel EE, et al. Bilateral (acute) hydronephrosis mimicking polycystic renal pathology. MOJ Anat Physiol. 2017;4(4):344–346. DOI: 10.15406/mojap.2017.04.00144
Complete or partial urethral obstruction results in progressive nephropathy in the subsequent calyxal and renal parenchymal damage. We report a case controlled giant hydronephrosis mimicking multiple polycystic kidney disease (PCKD). The fluid content in the collecting duct is about 1.4liters.
A 40years old man with renal dimensions measuring RK: 118x62mm; LK: 120x65mm respectively reported for ultrasound examination. There was no evidence of malignancy after 8-month follow-up ultrasonography with drug treatment in the internal medical unit; plus urologic evaluation and documentation. Expelled urinary volume via catheter was consistently measured.
Although clinical symptoms and alternate list of diagnosis were suspected, it turned out to be a case of large hydronephrosis. Accurate diagnosis became challenging due to distortion of renal parenchyma and calyxal atrophy. Examining clinical presentations, real-time sonogram evaluation and treatment medication, it is concluded that ureteric calculus may be a main cause of bilateral hydronephrosis.
Keywords: hydronephrosis, cysts, ultrasound, catheter
According to Mergener et al.1 Benign Prostatic Hypertrophy (BPH) accounts for increased incidence of hydronephrosis in males, while it is likely due to cyesis or endometriosis in females. Hydronephrosis refers to dilation in the calyx and renal pelvis near region of constriction in the urinogenital tract. This may or may not be associated with abnormal pyramidal pathology as the site of obstruction to urine passage indicates bilateral or unilateral hydronephrosis.2
Occurrence of giant hydronephrosis is rare and usually contains about 1.8litres of fluid in the ductules. Polyuria associated with hydronephrosis seems correctable through interactional (and non-surgical) means. It is well documented that3 the practice of non-surgical management/reduction of Pelvi-Ureteric Junctional (PUJ) obstruction may potentially reducing the number of premature renal uropathies.
In 2004, Lewis et al.4 concluded that retrospective Ball on dilation is an effective treatment method for PUJ obstruction with long term alleviating effect. The adverse effect of an aquaretic drug (polyuria, nausea and thirst) will interrupt the lifestyle of some patients. However, subjects at risks of rapid progressive hydronephrosis might prefer treatment with an aquaretic-drug and endure its side effects. Drugs capable of interfering with water hemostasis should be avoided as should anticholinergic medications with known undesired ability to limit bladder contractability.5
From literature, 2 in 10 patients undergoing dialysis have polycystic kidney disease (PCKD), with increased renal hypertrophy by a factor of 4.3 with partially impaired kidney function.
Though a common occurrence, complete or partial urethral obstruction produces a progressive damaging (reverse) renal pathology in the excretory kidney function. Multiple foci/stones or calculi may form if proliferation or infection occurs with subsequent impaired urination and kidney parenchymal destruction.6,7
This clinical observation was made at the Department of Radiology, Crystal Specialist Hospital (CSH) Akowonjo-Lagos, Nigeria. A male patient with hydronephrosis related (but not limited) to PUJ obstruction, stricture of the ureter negated (oral history) of symptoms like weight gain or loss, fever, increased temperature and fatigue.
Sonographic confirmation of hypertrophied but ‘polar’ kidneys; similar to embedded renal cysts with predominantly low echogenicity and multiple sonopenic fluid spaces (Figure 1&2). A General Electric (GE) Pro-Logic 3 ultrasound machine (made in the USA) with a 3.5 MHz curvilinear transducer was used for scanning. There was no sonic evidence of malignant disease. Informed consent of patient was obtained and ethical approval was granted by CSH in line with the 1975 reviewed Helsinki Declaration on confidentiality and patient-rights. Prior to the diagnosis of hydronephrosis, fasting for 6 hours and dehydration test was made. Recent history review through oral discussion with patient and medical case-note revealed compulsive and excessive water intake about 5 years ago (Table 1).
Nocturnal Urination |
Daytime Micturition |
Total Daily Diuresis |
1895 ± 163 ml |
6138 ± 349 ml |
8168 ± 257 ml |
2576 ± 402 ml |
2500 ± 630 ml |
471 ± 125 ml |
Table 1 Gauged urine quantity (via in-situ Foley’s Catheter)

Figure 1 Acute hydronephrosis of the RT kidney (K) with cystic-like corticomedullary differentiation, note isolated dilation of the renal pelvis.
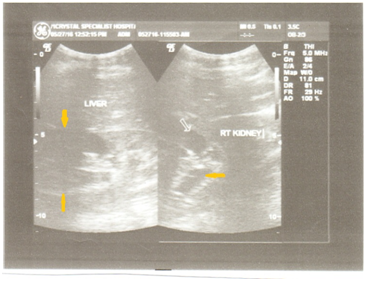
Figure 2 (Ultrasound B-mode split image) RT kidney with possibility of refluxing primary mega-ureter. Progressive renal failure can occur even after treatment due to abnormal physiologic bladder function. Note the arrow pointed downwards.
By July 2016 (see sonograms), no reflux in patient was observed post-micturition cystography. At present, December 2016, after follow-up presentation for ultrasound, increased urination averaging 29 times/day, with stable kidney function; serum creatinine: 1.48 mg/δl. Though some patients have undergone surgical procedure to alleviate functional obstruction,8 it is advisable treatment is medical. Instruction to patients on the importance of early frequent voiding cannot be overemphasized. The RT kidney (Figure 1) measured 118 x 62mm in longitudinal and AP diameters, LT kidney (Figure 3&4) dimension was 120 x 65mm before progression.
Hydronephrosis caused by PUJ impairment formed approximately 38% of our previous study before this case report. Most of the patients who earlier came with symptoms to (CSH) were in the late teen-age group. On physical palpation subjects had tenderness and resistance in the lumber region, accounting for 88% of patients. A study9 in 2001 carried out pyeloplasty in 56 cases over a decade and concluded that the procedure is an excellent innovation for PUJ obstruction and produces clear urinary tract drainage. Although ill patients have undergone surgical procedure to alleviate functional tract obstruction8 we suggest treatment is made medical. Multiple dilated calyces (Figure 1), loss of corticomedullary differentiation, renal dysplasia and increased parenchymal echogenicity are all anatomical landmarks in-situ of the diseased kidneys.
Social inconvenience of frequent voiding e.g. in an airplane, makes sufferers adopt self-urinary retention which further exacerbate chronologic uropathy in line with the findings of Boyd et al.10 Furthermore, cases of moderate (non-acute) dilation may resolve with time. In severe persistent hydronephrotic kidneys, a long-term sonar follow-up is required because of the possibility of late worsening. It (hydronephrosis) can be further graded into severe, mild or moderate according to AP diameter of the kidneys based on observed sonogram pathology. Time frame for recurrence can vary from a few months to within a 3year period.
Improved medication after a short period of time can lead to marked improvement in kidney tract dilation, if diagnosis by ultrasound is made early. Chronic renal failure rarely occurs11 however, persistent hydronephrosis presumably of many years can be improved and managed in line with the assertion of Tank et al.,12 Singer et al.,13 followed up stented patients; concluding medical management is of great value in the early detection of morbidity and other complications of hydronephrosis. Prolonged and sustained polyuria (diuresis >30/day) is usually a cause of reduced tubular fluid resorption and obstructed uropathy in some patients. This is similar to an earlier literature reporting by Drach.6 Multiple dilated calyces and loss of corticomedullary differentiation (Figure 1) and partial increased parenchymal echogenicity are all anatomical landmarks in-situ of the diseased kidneys.
Physical impairment to urine flow results in the disruption of glomerular hemodynamics and tubular function, caused by a variety of vasoactive factors. However; hematuria, resistance in the lumbar area (on palpation), low abdominal pain and urgency in urination are associated symptoms. Endoscopy combined with pressure-releasing surgical procedure should be used in managing nephrological interventions. In severe cases, thickness of renal parenchyma should be determined during scanning.
Treatment drugs with aquaretic side effects (polydipsia, polyuria, nocturia and thirst) were associated with increased level of uric acid and gout. Compared with patients who received placebo, the rate of increase in kidney volume was low in both study groups (2.8% per year in toluaptan and 5.5% per year in placebo) contrasting to 10% per year in other studies.14‒16 If abnormal bladder function combine with acute hydronephrosis progressive renal failure may occur.
There are obvious limitations in viewing renal vasculature (of hydronephrotic kidneys) with grey scale ultrasound in this case report. Color Doppler evaluation will further differentiate between non-obstructive and obstructive hydronephrosis. Renal-foci, streaks of calcification and ureteric calculus can be a cause of hydronephrosis when seen.
None.
Non-declared, the case note is self-sponsored.

©2017 Moyosore, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.