Journal of
eISSN: 2379-6359


Research Article Volume 9 Issue 3
1Rinofast Polanco, Mexico
2Clinica BAU, Spain
3Corporodo Clinic, Colombia
Correspondence: Alberto Candau-Alvarez, C/ Poeta Jose Maria Alvariño 22 CP: 14012 Cordoba, Spain, Tel +34 647769528
Received: November 06, 2017 | Published: December 8, 2017
Citation: Marin HM, Candau-Alvarez A, Duran JE (2017) Easy Recognition of Caudal Lower Cartilage Rim Localization for Marginal Incision in Tumescent Rhinoplasty. J Otolaryngol ENT Res 9(3): 00290. DOI: 10.15406/joentr.2017.09.00290
Nasal tumescence with local anesthetics is a technique that allows a complete rhinoplasty without the need of general anesthesia, minimizing the bleeding and optimizing the recovery of the patient. Besides these benefits, the natural distorption of the tissues the tumescent solution creates shows new anatomical landmarks, which is the case of a fold that localizes the lower cartilage rim. This fold is not appreciate in non-tumescent rhinoplasty approach. In this article, we discuss the role of tumescent anesthesia to facilitate the dissection of the lower cartilage rim in the marginal approach through this mentioned fold. This easy location made that complete lower cartilage rim dissection can be completed in a significantly reduced time (p=0.001), but it does not decrease the risk of cartilage injury in an experimented hands.
Keywords: rhinoplasty, dissection, nasal cartilages, esthetics, nasal septum
LCRD, lower cartilage rim dissection; LCR, lower cartilage rim
Hydrodissection is described as a useful technique in many surgical areas. Reasons for that mainly include easy surgical dissection, less bleeding due to vasoconstrictors and the vessel compression the tumescence does itself, decrease postsurgical pain and improves patient recovery. However, in nasal surgery only few articles cite the use of this technique.1,2
The tumescence expose new anatomical landmarks consequence of the uneven tissue distortion after fluid injection. Marginal incisions are described by many manners: while some authors use metrical distances,3,4 others use anatomical landmarks,5 or direct palpation,6,7 which is difficult in thick skin patients. In this paper, we describe a new anatomical landmark that appears after tumescence rhinoplasty technique and how this fold affects to the surgery in terms of reducing operative time.
We conducted a retrospective study in patients to whom an aesthetical primary closed rhinoplasty procedure was done between May 2015 and May 2017 (24months). The two compared groups was the tumescent rhinoplasty technique (n= 8 patients) as explained above, and the non-tumescent rhinoplasty technique, mentioned as “normal” technique (n= 6 patients). The group assignation was done based on the desire of the patient to be operated with local anesthetics only, or under general anesthesia. This randomization was not related to the nasal anatomy nor previewed difficulty. All patients were operated by the same surgeon (A.C-A). The technique of the tumescent rhinoplasty used is described below.
The main variable was the time in lower cartilage rim dissection (LCRD, measured in minutes) and the cartilage rim injury due to the approach (defined as any non-expected injury of the lower cartilage during the exposition because an incorrect location of the caudal border of the cartilage) measured on a binary option “Yes” or “No”. Other variables as age and sex were measured. Although each patient had a different surgical planning, in every patient the dissection of the lower cartilage rim was constant.
Because the small sample size, the statistical analysis was done using two-tailed Mann-Whitney-U test for continuous variables (Time in LCRD), and Chi-square with Yate´s correction for dicotomical variables (Cartilage Injury). Mean and range of all continuous variables were also expressed.
Surgical technique
The procedure starts with the injection of local anesthetics at nasal area. We use lidocaine 2% with epinephrine 1:10000 into standard Carpule vial of 1, 8mL to perform the tumescence. The mean of cartridges we use to inject is 11 per patient. The infraorbital nerve blockade is the first injection point, followed by the anterograde injection starting from the columella and tip of the nose, advancing trough the radix. Then, the lateral cartilages and the nasal bones are anesthetized percutaneously. Finally, the septum is injected at both sides in a framework fashion of three arrows with three injection points.
The marginal incision is helped with a double-sharp point retractor with a vertical vector. Digital counter-pressure of the nasal ala is helpful (Figure 1).

Figure 1 Technical description. (A) The surgeon´s position is crucial to evidence the fold. The Joseph twin retractor is placed vertically, 45º degrees of inclination from the patient stand position, and a gentle digital pression is done with a finger to expose the internal aspect of the nasal fossa. (B) The fold reveals the exact position of the caudal rim of the lateral cartilage, without risk of injury nor bleeding. (C) In non-tumescent rhinoplasty is hard to demonstrate the fold, as it is easily recognized after the hydrodissection done by the tumescence (D).
At this point, a fold is seen at the internal aspect of the nasal fossa. With a no. 15 blade, we incise in the middle of that fold all long until communicate with the medial incision below the filtrum. After that, we dissect a small pocket in the middle of the incision with a sharp Converse scissors, and finally we complete the dissection cutting along the incision with a blunt tip Converse scissors (Figure 2).
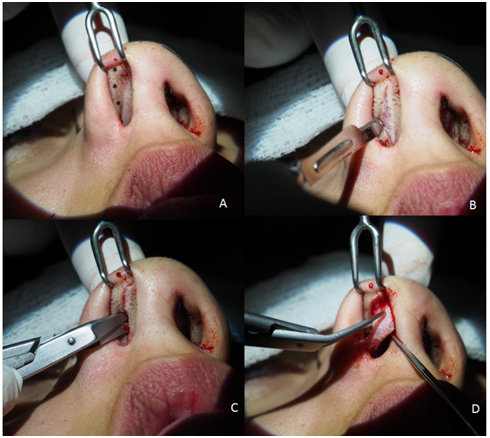
Figure 2 Technical description. (A) After tumescence, the lower cartilage rim is depicted by the fold (*). (B) In the middle of the fold we incise the nasal aspect of the skin longitudinally without passing through the submucosa. (C) With the Sharp Converse Scisssors we dissect a small pocket through the subcutaneous layer. (D) Finally, with the Blunt Converse Scissors we dissect and cut safely and easily the alar cartilage from the upper side.
Results
Six male patients (42.85%) and 8 female patients (57.15%) were enrolled in the study. Mean age was 30.57 years (Range 22-43years). All the patients received aesthetic primary closed rhinoplasty (Table 1). The statistical analysis revealed that tumescent technique allows a statistically significant faster dissection (Table 2), although in an experimented hands the risk of lower cartilage rim injury do not decrease (p>0.05) (Table 3).
Patient |
Group |
Age |
Sex |
LCRD (Minutes) |
Injury |
Approach |
1 |
Normal |
24 |
M |
36 |
Yes |
Closed |
2 |
Normal |
29 |
M |
40 |
No |
Closed |
3 |
Normal |
40 |
F |
45 |
No |
Closed |
4 |
Normal |
34 |
M |
40 |
No |
Closed |
5 |
Normal |
29 |
F |
30 |
Yes |
Closed |
6 |
Normal |
32 |
F |
47 |
No |
Closed |
7 |
Tumescent |
34 |
M |
25 |
No |
Closed |
8 |
Tumescent |
22 |
M |
21 |
No |
Closed |
9 |
Tumescent |
30 |
F |
20 |
No |
Closed |
10 |
Tumescent |
31 |
F |
36 |
No |
Closed |
11 |
Tumescent |
25 |
F |
30 |
Yes |
Closed |
12 |
Tumescent |
43 |
F |
20 |
No |
Closed |
13 |
Tumescent |
26 |
M |
31 |
No |
Closed |
14 |
Tumescent |
29 |
F |
22 |
No |
Closed |
Table 1 Population and variables collected
LCRD: Lower Cartilage Rim Dissection; M: Male; F: Female; Injury, Any non-expected injury of the lower cartilage during the exposition because an incorrect location of the caudal border of the cartilage
|
Time in LCRD |
|
|
|
Mean |
SD |
p Value |
Tumescent Technique |
25,63 |
6,02 |
0,001 |
Normal Rhinoplasty |
39,66 |
6,15 |
0,001 |
Table 2 Mann-Whitney U test for the continuous variable (time spent in lower cartilage rim dissection)
LCRD: Lower Cartilage Rim Dissection; SD: Standard Deviation. Values of p>0,05 are consider non-significant
|
Injury of LCR |
|
|
|
Yes |
No |
p Value |
Tumescent Technique |
1 |
7 |
0,77 |
Normal Rhinoplasty |
2 |
4 |
0,77 |
Table 3 Chi-Square test with Yate´s correction for the 2x2 contingency table of the risk of injury during the approach to the alar cartilage
LCR: Lower Cartilage Rim. Values of p>0,05 are consider non-significant
The described anatomical landmark allowed the surgeon to dissect the alar cartilage faster but it does not increases the safety as the risk of injury was not significantly different.
Discussion
The exact location of the lower cartilage rim edge is crucial for an exact dissection, and its correct location requires expertise and also the knowledge of the anatomy. Some clinical and cadaveric studies describes a mean distance of 6,7mm from the skin rim to the caudal border.8 Kamburoğlu et al.,4 set the marginal incision 3-4mm from the skin rim regardless the cartilage can be some millimeters ahead. A cadaveric study sets the variable distancies that can be observed among patients 5. Direct palpation is technically a challenge because of the expertise the surgeon needs to have. A 1752 rhinoplasty study made by Akbas et al.,6 about the management of the lateral cartilages used direct palpation to localize the caudal edge to set the marginal incision. Other author preferred the location based on the anatomical landmarks as is the piriform aperture.9
The hydrodissection in rhinoplasty surgery is a current trend. Saline tumescence could be consider as the reference solution injected, but in our patients we used lidocaine with vasoconstrictor as described above. Gungor et al.,10 denied the benefits of anesthetic tumescent rhinoplasty. However, in his study he concludes that there was no benefits in terms of bleeding decrease or mucosal injury prevention, in our opinion it concedes us the possibility to do a complete rhinoplasty only with local anesthetics, which is impossible otherwise if normal saline is only injected. Vanniasegaram11 consider in his prospective study of the use of vasoconstrictors versus saline in septal surgery, that there is no benefits of using adrenaline, without dramatic differences in blood loss and operative time between the two groups. McClymont et al.,12 consider the using of local anesthetics with vasoconstrictors an optimal combination for septal surgery. In our opinion, the risk of bleeding is higher in non-tumescent rhinoplasty. Until the present, we reported no ischemic necrosis nor vascular disturbances at nose skin due to the vasoconstriction.
Dubach et al.,13 described in a cadaveric specimen the different planes in which the tumescence can facilitate the dissection, being the subperichondrial plane the harder to achieve in comparison with the supraperichondrial plane, which could be inconsistent with the concept of the hydrodissection as a helpful technique for flap dissection. Although there is no other methodologically similar anatomical study to contrast the results, the authors agree that the tumescence the hydrodissection do helps itself the rhinoplasty surgery, as other authors have been reported.2
The fold here described allows us to identify the caudal border of the lower cartilage in tumescent rhinoplasty. There is no evidence, to the best of our known, of previous description of this anatomical landmark, which is only evident after tumescence of the nose. The uneven dilatation and distortion capability of the nasal lower cartilage tissue is the best explanation of this phenomenon. This surgical tip allows us to perform a complete alar cartilage dissection in a significant lower time than in the normal rhinoplasty. However, this tumescent technique does not decrease the cartilage damage risk itself. Further anatomical and histological studies are needed to clarify the nature of this fold.
We recognize the helpful role of Dayanira Trinidad MD, Sergio Contreras MD, Ivan Perez MD, Oscar Barbosa MD, Jose A Gallegos MD, Lourdes Galvan MD and Yader Guzman MD in the development of this paper.
Authors hereby declare no financial disclosure or conflict of interests about the contents of this article.
None.

©2017 Marin, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.