Journal of
eISSN: 2373-4345


Background: The use of Zirconia abutment is increasing in the search of an aesthetic rehabilitation.
Purpose: The purpose of this in-vitro study was to assess the bending moment and fracture patterns of different types of zirconia abutments with internal hexagonal connection and as well as to compare their respective bending moment to those internally connected titanium abutments.
Materials and methods: Forty-eight analog abutments were prepared for 6 groups with 8 samples each (AT Group: Alpha Bio Titanium abutment; AZ group: Alpha Bio Zirconia abutment; BT group: Biohorizons Titanium abutment; BZ group: Biohorizons Zirconia abutment; ZT group: Zimmer titanium abutment; ZZ group: Zimmer Zirconia abutment). Samples were subjected to static compressive load applied at 30-degree angle to the axis of the abutment-analog complex in the palatal surface, using a universal testing machine at 1.00mm/min speed until fracture occurred, or after a decrease of 20% of the load applied if the fracture was not observed. One-way ANOVA, Turkey HSD test and t-test were used for statistical analyses (α=.05).
Results: The mean (SD) bending moments of the titanium abutments were for Alpha Bio 374.4±50.74 Ncm; for Bio Horizons 271.7±31.72 Ncm and for Zimmer 193.6±23.83Ncm. There were significant differences among them (α= .0001, Tukey HDS test). The mean (SD) bending moments of the Zirconia abutments were for Alpha Bio 295.8±77.5Ncm; Bio Horizons 269.9±61.7 Ncm and for Zimmer 115.3±23.37Ncm. Zimmer zirconia abutments showed a significant lower bending moment as compared to Alpha Bio and Biohorizons zirconia abutments (α= .0001,Tukey HSD test). The type of fracture of zirconia abutment observed was strongly related to the type of secondary metallic element.
Keywords: implant, abutment, zirconia, titanium, bending moment, fracture
AT, alphabio titanium; AZ, alphabio zirconia; BT, biohorizons titanium; BZ, biohorizons zirconia; ZT, zimmer titanium; ZZ, zimmer zirconia; SD, mean; M, moment; HSD, honestly significant difference
The replacement of missing anterior tooth with an osseointegrated implant or with a fixed dental prosthesis is part of the routine practice of today dentistry resulting in treatment with high success rates.1 Titanium abutments are the gold standard in rehabilitation of implants in cases of fixed prosthesis, due to their excellent biologic properties and great biomechanics characteristic. However, metal abutment cause discoloration of the peri-implant mucosa because of its gray color.2,3 putting in risk the esthetic outcome. Taking this problem into account, different ceramic abutments made of zirconia, alumina or other ceramic materials are now available.4
The use of ceramic abutments offers several clinical advantages over metallic abutments. The esthetic outcome is not only related to the similarity of the color peri-implant mucosa between a natural tooth and a zirconia,5 but also with the easiness in manage the color outcome of all ceramic fixed prosthesis.6 In addition, the biologic properties of zirconia are similar or even better than titanium,7 showing low in-vivo bacterial adhesion,8–10 less peri-implant inflammation,11 and even soft tissue integration.12,13
Implants have different designs of implant abutment connection and the connection of the zirconia abutments to the implant can be carried out by means of the abutment itself or through a secondary metallic element. Several investigations have indicated that the fracture resistance of a ceramic abutment is dependent of the type of implant abutment connection and the presence of a secondary metallic element,14–17 However, in the current research there is a lack of studies regarding the difference on the fracture resistance of zirconia abutments with different combinations of secondary metallic elements, using an internal hexagon connection.
The working hypothesis was that the presence of a secondary metallic element increases the fracture resistance of the zirconia abutment with internal hexagonal connection.
The aim of this in-vitro study was to assess the bending moment and fracture patterns of different types of zirconia abutments with internal hexagonal connection and as well as to compare their respective bending moment to those internally connected titanium abutments.
A total of 48 abutments were studied. They were divided into six groups (n=8 each). Three types of zirconia abutments were tested: group AZ consisted in a zirconia abutment that was connected to the implant through a titanium base that did not allow the zirconia to have any contact with the implant itself (Alpha Bio, Petah Tikva, Israel), group BZ that did not have any secondary metallic element (Bio Horizons Implant Systems, Birmingham, AL, USA), and group ZZ that consisted in a solid zirconia body with a titanium seating ring that serves as an interface between the zirconia abutment and the ledge of the internal hexagon connection (Zimmer Dental, Carlsbad, CA, USA). The other three groups were titanium abutments: AT group (Alpha Bio, Petah Tikva, Israel), BT group (Bio Horizons Implant Systems, Birmingham, AL, USA) and ZT group (Zimmer Dental, Carlsbad, CA, USA). In Tables 1 & 2 all the characteristics of the implant components tested are summarized.
Characteristic |
AlphaBio |
BioHorizons |
Zimmer |
Abutment length |
8.5 mm |
8 mm |
8.5 mm |
Implant-abutment connection |
Internal hexagon |
Internal hexagon |
Internal hexagon |
Analog material |
Stainless steel |
Titanium alloy |
Titanium alloy |
Abutment configuration |
OTST |
OTST |
OTST |
Table 1 Titanium abutment components tested
OTST, One-piece with titanium screw
Characteristic |
AlphaBio |
BioHorizons |
Zimmer |
Abutment length |
10.5 mm |
7 mm |
7 mm |
Implant- Abutment connection |
Internal hexagon |
Internal hexagon |
Internal hexagon |
Analog material |
Stainless steel |
Titanium alloy |
Titanium alloy |
Secondary component |
Titanium connection |
None |
Titanium ring |
Screw material |
Titanium |
Titanium |
Titanium |
Table 2 Zirconia abutment components tested
The preparation of samples was performed embedding the analog in a self-cure acrylic (Melio Dent, Heraus, Kulzer, Hanau, Germany) cube using custom-made positioning device to standardize the position of the analog. The axis of the analog was positioned in 30° respect to the vertical axis according to the ISO-Norm 14801.18 The acrylic was at the same level of the top of the analog so no vertical bone lost was simulated. Then the abutments were fixed on their respective analog with the torque values (30 Ncm for all group) as recommended by the manufacturers by means of an electronic torque motor (Osseoset 200, Nobel Biocare, Gothenburg, Sweden).
The samples were subjected to a static compressive load applied at 30° angle to the axis of the abutment-analog complex in the palatal surface, using a universal testing machine (Model 4467, INSTRON Corp, Norwood, MA, USA) (Department of Materials Engineering, University of Concepción, Concepcion, Chile) at 1.00mm/min speed until fracture occurred, or after a decrease of 20% of the load applied if the fracture was not observed. The force recorded by the machine in all procedures was performed by a single investigator.
For comparison of fracture resistance for all the groups, the bending moment (M) was calculated in Ncm according to the formula M=0.5 x F x L (ISO Norm 14801), 18 with the F being the load (N) and L being the vertical distance from the simulated bone level to the center of the load (cm).
Abutment fracture types were divided into: fractures above and below the analog shoulder. If the fracture was above the analog shoulder, both complete fractures and cracks were differentiated. In addition, the failures and deformation of analogs and screws were recorded. All specimens were photographed (Nikon D40, Micro Nikkor 60mm AF-D Tokyo, Japan).
The bending moments were used for the statistical comparisons of the groups. Data were tabulated and statistical tests were performed with SPSS Program 16.0 (SPSS Inc., Chicago, IL, USA). Kolmogorov-Smirnov test was used to evaluate the normal distribution of the data. Differences among groups were examined by means of a t-test, and one-way analysis of variance ANOVA followed by Turkey Honestly Significant Difference (HSD) multiple comparison test (α=.05).
The normality of the data was verified by means of Kolmogorov-Smirnov test, which revealed a normal distribution of the bending moment values.
Bending moments
The mean (SD) bending moment for groups of titanium abutment (AT, BT and ZT) was 279.93±83.55 Ncm and in the groups of zirconia abutment (AZ, BZ and ZZ) was 227.05±98.86Ncm (Table 3).
Material |
Manufacture |
Mean(Ncm) |
SD |
Titanium |
AlphaBio |
374.40 |
50.74 |
Biohorizons |
271.76 |
31.72 |
|
Zimmer |
192.63 |
23.84 |
|
Zirconia |
AlphaBio |
295.84 |
77.53 |
Biohorizons |
269.94 |
61.69 |
|
Zimmer |
115.37 |
23.18 |
Table 3 Bending Moments (Individual values, means and standard deviation; in Ncm) for titanium and zirconia abutments
Data showed that when the bending moments of titanium and zirconia abutments of the same manufacture were compared, a significant difference was only observed in Zimmer group in which the bending moment of the titanium was higher that the zirconia abutment (α=.0001, t-test).
For the comparison of titanium abutments (AT, BT and ZT) the one-way ANOVA revealed a significant difference among the mean bending moment values of the three groups (Table 4). When a post-hoc test was applied to compare all the titanium groups showed significant differences among AT, BT and ZT (α=.0001, Tukey HSD test). These data are presented as a box plot in Figure 1.
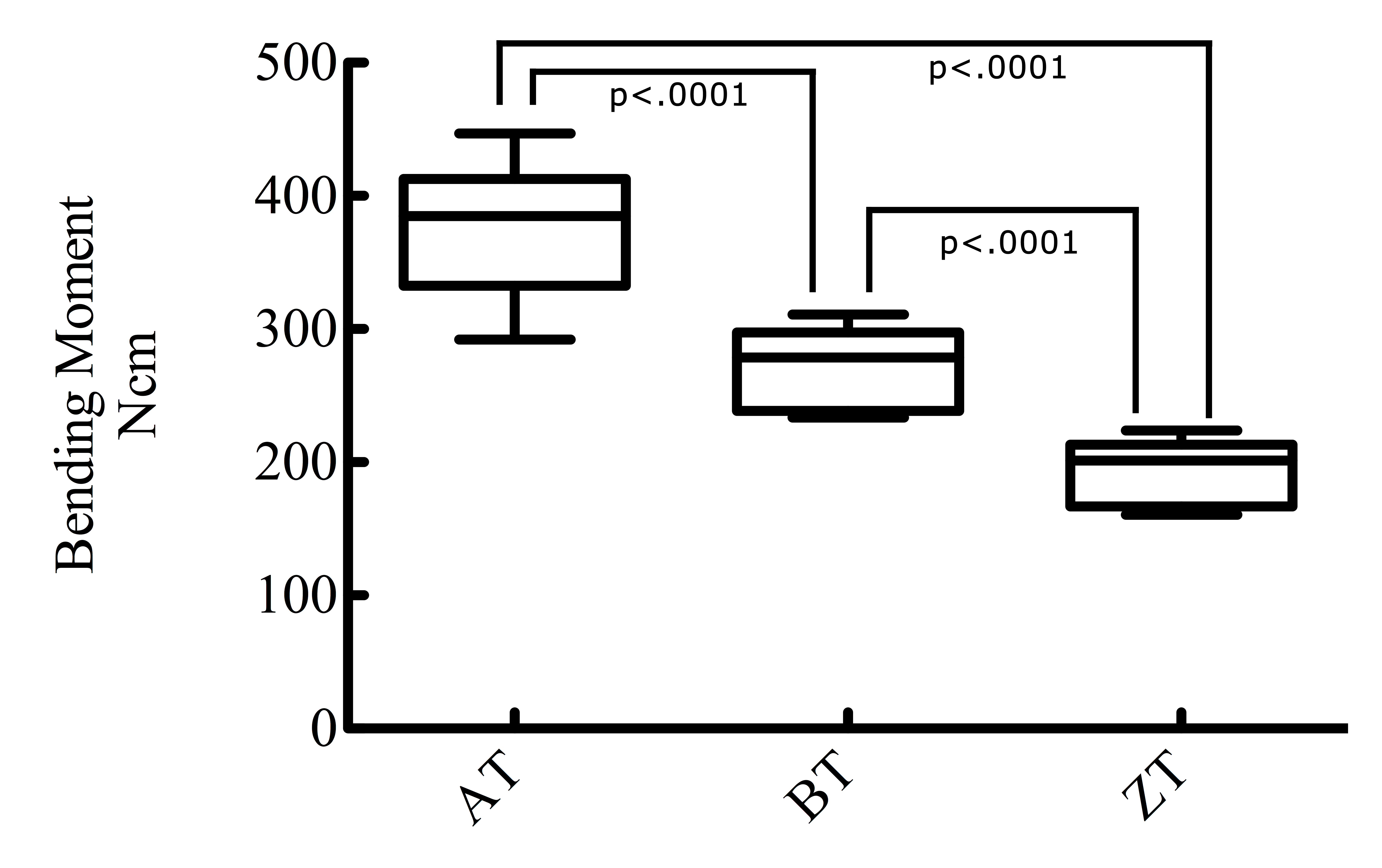
Figure 1 To compare all the titanium groups showed significant differences among AT, BT and ZT (α= .0001, Tukey HSD test).
Material |
|
Sum of Squares |
df |
Mean Square |
F |
P |
Titanium |
Among Groups |
131511.37 |
2 |
65755.68 |
47.54 |
.000 |
Residual |
29046.03 |
21 |
1383.14 |
|||
Total |
160557.40 |
23 |
||||
Zirconia |
Among Groups |
152347.58 |
2 |
76173.79 |
22.07 |
.000 |
Residual |
72479.12 |
21 |
3451.38 |
|||
|
Total |
224826.75 |
23 |
|
|
|
Table 4 Result of one-way ANOVA for bending moment of Titanium and Zirconia abutments
Df, Degrees of Freedom; F, F-test
In the group of zirconia abutments (AZ, BZ and ZZ), the one-way ANOVA exhibited a significant difference among the values of the three groups (Table 4). Post-hoc Turkey HSD multiple comparison test, applied to bending moments in zirconia abutments detected significant difference among AZ and ZZ, and BZ and ZZ (α=.0001), but no significant difference (α=.685) was detected between AZ and BZ groups (Figure 2).

Figure 2 Bending moments in zirconia abutments detected significant difference among AZ and ZZ, and BZ and ZZ (α= .0001), but no significant difference (α= .685) was detected between AZ and BZ groups.
Failure types
The most common failure in all groups (Titanium and Zirconia) was the screw deformation (72.9%). The failure types of the specimens are described in Table 5.
Manufacturer |
Fracture Below Analog Shoulder |
Screw Deformation |
Fissure |
Fracture Above Analog Shoulder |
Analog Deformation |
Hexagon Deformation |
||||||
Nº |
% |
Nº |
% |
Nº |
% |
Nº |
% |
Nº |
% |
Nº |
% |
|
AlphaBio Titanium |
0 |
0 |
8 |
100 |
0 |
0 |
0 |
0 |
0 |
0 |
8 |
100 |
AlphaBio Zirconia |
0 |
0 |
4 |
50 |
2 |
25 |
5 |
62.5 |
0 |
0 |
0 |
0 |
Biohorizons Titanium |
0 |
0 |
8 |
100 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
Biohorizons Zirconia |
8 |
100 |
7 |
87.5 |
0 |
0 |
6 |
75 |
0 |
0 |
0 |
0 |
Zimmer Titanium |
0 |
0 |
8 |
100 |
0 |
0 |
0 |
0 |
8 |
100 |
0 |
0 |
Zimmer Zirconia |
0 |
0 |
0 |
0 |
0 |
0 |
8 |
100 |
0 |
0 |
0 |
0 |
Table 5 Failure types after static force test (samples per group 8)
In the groups AT and ZT all the samples exhibited bending of the screw. Plastic deformation of the hexagon located in the abutment (Figure 3) was observed only in group AT and plastic deformation of the analog only in the group ZT (Figure 4).
In general, in the titanium abutments groups (AT, BT and ZT) the main failure was deformation of a component of the assembly, either the abutment or the analog. On the other hand, in the groups of zirconia abutments (AZ, BZ and ZZ), the fracture of the zirconia abutment itself was the primary cause of failure.
In the groups of zirconia abutments (AZ, BZ and ZZ) the majority of them presented failure above analog shoulder (fracture or fissure) (79.1%). The fracture below the analog shoulder was observed in all the samples of group BZ (100%), interestingly this type of failure was seen exclusive in this group (Figure 5).
In the present in-vitro study, the bending moments and fracture patterns of different types of titanium and zirconia abutments, both with internal hexagonal connection were studied. Our results indicate that the bending moment of titanium abutments compared to zirconia was significant higher. This is in agreement with the findings in previous studies.15–17,19 In addition, the titanium abutment exhibits significant higher bending moment than zirconia of the same manufacture, except those ones of Zimmer groups in which there was no different among them.
In the groups of zirconia abutments, the higher mean bending moments was for the group AZ with 295.83±77.5 Ncm, BZ 269.9±61.7 Ncm, and ZZ with 115.37 Ncm. The Zimmer zirconia abutments showed a significant lower bending moment as compared to Alpha Bio and Biohorizons zirconia abutments. However, no significant difference was detected between AZ and BZ groups. These results are in accordance with previous studies, where it has been shown a similar range of bending moment of zirconia abutments.14–16
The presence of a secondary metallic element such as titanium seating ring in ZZ abutments did not increase the bending moment. Otherwise, in the group AZ, zirconia abutments were connected to the implant through a titanium base that did not allow the zirconia to have any contact with the implant. From the results of the present in-vitro investigation, this type of secondary metallic component exhibited higher mean bending moments than any of the tested zirconia abutments. This data leads us to partially reject the working hypothesis. One possible explanation for this may be that the secondary metallic element such as the seating ring is weaker than the design of secondary metallic component of the Alpha Bio Zirconia abutments.
Several studies have provided evidence in order that the zirconia abutments with a secondary metallic element exhibit higher bending moment, but the comparison was performed among different types of implant abutment connection.14–16 Our results are consistent with the findings in a study by Kim et al.20 who found that the use of a metallic element with a zirconia abutment does not guarantee higher fracture resistance.
The most common failure in all groups Titanium and Zirconia was the screw deformation, this is in agreements with other reports.17–19 In the group of Alpha Bio titanium all the specimens showed screw and hexagon deformation and no deformation were detected in the analogs. This was also seen by Sundh et al.21
In zirconia abutments groups, the most typical fracture pattern was fracture above analog shoulder.22 This findings, which confirms observations from others studies.15,16 The fracture below the analog shoulder was observed only Biohorizons zirconia abutments and in all its specimens, this is a common failure reported in zirconia abutment without a secondary metallic element.17,23,24 It may therefore be assumed that the fracture patterns are strongly associated with the presence and type of secondary metallic element in zirconia abutments with internal hexagonal connection.20
Further clinical studies should be carried out in other to evaluate these findings, because the most important of such findings is the long term success of the zirconia abutments on implants.
Within the limitation of this in-vitro study, the following conclusions can be drawn:
The bending moments after static loading of titanium abutments of Alpha Bio, Biohorizons and Zimmer revealed significant difference.
Titanium abutments exhibited significantly higher bending moments compared to Zirconia abutments only in the Zimmer group.
The bending moment of the zirconia abutment with a secondary metallic element depends of the design of this element.
The use and type of metallic secondary component in the zirconia abutment influence the failure behavior.
None.
The authors thank Alpha Bio Tec, Biohorizons and Zimmer Dental for their support in term of implant components and the Department of Materials Engineering, University of Concepción, Concepción, Chile for their support.
Authors declare that there is no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.