Journal of
eISSN: 2373-4345


Purpose: The purpose of this study was to evaluate the effect of alveolar corticotomies on anchorage loss by comparing and measuring the amount of anchorage loss with titanium mini-screws and conventional molar anchorage during anterior segment retraction.
Materials and methods: In this study, we compared treatment outcomes of patients with severe class ІІ malocclusions treated using mini screw anchorage (n=8) or traditional orthodontic mechanics of inclusion of the second molars (n=8). Both methods were combined with alveolar corticotomies before retracting the anterior segment. Pretreatment and post treatment lateral cephalograms were analyzed.
Results: Both treatment methods achieved acceptable results as indicated by the reduction of overjet. The mesiodistal position of the maxillary molars in group2 showed a small change (+1.5mm).
Conclusion: Alveolar corticotomies on the anterior teeth combined with inclusion of second molars proved to be efficient for intraoral anchorage reinforcements for en-masse retraction of the maxillary anterior teeth.
Various treatment techniques and biomechanical approaches have been suggested over the past decades to achieve en-masse retraction of anterior teeth with minimal or no anchorage loss.1,2 Anchorage has been classified based on the magnitude of mesial movement of the posterior teeth during anterior retraction.2
Minimal anchorage results in extraction space closure primarily by mesial movement of the posterior teeth. Moderate anchorage is often described as reciprocal movement of anterior and posterior teeth in to the extraction sites. To reinforce anchorage, various auxiliaries can be used, including headgear, lingual arch, trans palatal arch and inter maxillary elastics.3
The disadvantages of these appliances might be the need for patient compliance. However, improvement can be minimal because it is difficult to establish absolute anchorage for incisor retraction with traditional orthodontic mechanics such as including the second molar in treatment.4 Recently, mini-implants have been widely used to provide stationary anchorage for various tooth movements.5–10 More recently, the development of corticotomy-assisted orthodontics has provided new solutions to many limitations in the orthodontic treatment.11
Although corticotomy is an old technique dating back to the early 1900s, it was not properly introduced until Wilcko developed the patent technique named Accelerated Osteogenic Orthodontics (AOO).12,13 This technique was originally designed to enhance tooth movement, subsequently reducing treatment time via including cortical bone injury through linear cutting and then performing orthodontic treatment.11
However, the use of mini-screws is not always possible, be it for anatomical or financial reasons. This may be the best widow of opportunity for the use of alveolar corticotomies in orthodontics, i.e., when TADs cannot be used. No report has analyzed in detail the corticotomy-assisted orthodontic treatment results of class ІІ patients with traditional methods of anchorage. It is unknown if we can abandon the mini-screws in providing absolute anchorage when combining alveolar corticotomy in class ІІ malocclusion treatment.
The study design was a randomized controlled trial (RCT) (prospective study) with one observation subsequent to the initial baseline observation. Our subjects were 16 non growing patients from the orthodontic outpatient department (ages, 19-25; mean, 21.5 years, SD, 2.0) who met the following criteria:
Patients had skeletal class ІІ jaw-based relationships with ANB angle more than 5.0o, excessive overjet of more than 5.0mm, non growing, concerned about treatment time. On the basis of diagnosis of the presenting malocclusion, the extraction of the maxillary first premolars and retraction of the upper anterior teeth with maximum anchorage was indicated in all patients. We received informed consent from all patients, and they agreed to class ІІ camouflage treatment with premolars extraction combined with alveolar corticotomy to shorten the treatment time.
The subjects were randomly divided into two groups before treatment.
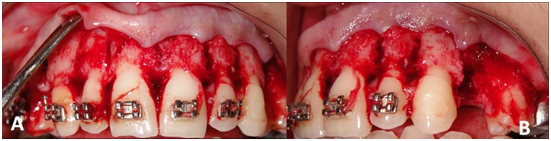
For all patients, Roth 0.022" pre adjusted edgewise appliance was used and the alveolar corticotomies were made before starting the retraction of the anterior segment. The corticotomy was carried out after the local anesthesia. A full thickness mucoperiosteal flaps were reflected both labially and lingually around all the upper of the anterior teeth (canine to canine), except for the lingual aspect of the inter dental papilla between teeth #8 and #9. Vertical bone cuts in the cortical bone were made about 1-2mm below the alveolar crest and were extended 2-3mm beyond the apices of the anterior teeth; these cuts were performed both facially and lingually from the distal of the right upper lateral incisor to the distal of the left upper lateral incisor with 1mm diameter ceramic bur (Komet, Germany). The cuts extended only about 1.5mm to the superficial aspect of the medullary bone, by confirming bleeding through the cut lines. After the extraction of the upper first bicuspids, ostectomies were performed at the site of the bicuspids, care was taken to extend the ostectomies as close as possible to the apices of the upper canines as possible without encroaching on the lining of the maxillary sinuses. Extensive bone thinning was performed on the distals of the canines leaving little more than the PDLs, lamina dura, and the thinnest layer of the medullary bone possible. The bone was thinned on the linguals of the upper canines and upper incisors. After bleeding control the flaps were repositioned and sutured in to place with interrupted loop 3-0 silk sutures (Figure 1).
In the (G1) patients, after leveling and alignment, mini-screws (Svenska Ortho-cut®, Sweden, diameter 1.6mm; length 1.8mm) were implanted in to the buccal alveolar bone between first molars and second premolars. After finishing the surgical procedure, a 0.019 x 0.025 inch St. St arch wire with anterior hooks was placed. Two weeks later, sutures were removed and Ni-Ti closed coil springs (Ortho Classic®; 6mm, extra heavy) were used from the maxillary mini-implants to the (8mm) hooks in the first group (Figure 2A).
In the second group the Ni-Ti closed coil springs were extended from the first molar's hook to the (4mm) hooks on the 0.019 x 0.025 inch St. St wire (Figure 2B). The six anterior teeth were retracted simultaneously with orthopedic forces of 450gr/side in both groups.14 All patients were examined at two weeks intervals for reactivation the retraction force until the overjet was resolved and a class І canine relationship was achieved. Lateral cephalograms at T1 (before treatment) and T2 (after retraction) were used for cephalometric analysis. Eight angular and two linear measurements were made to evaluate the skeletal and dental changes after orthodontic treatment (Figure 3). Two angular and two linear measurements were also made to evaluate the soft-tissue profile changes between T1 and T2.
A data base was created in the Microsoft Excel and statistical package for the social sciences (SPSS) version 13 was used for statistical analysis. The mean and standard deviation were calculated for each variable. Independent-samples t tests were used for comparison between the paired cephalometric variables at T1 and T2. A paired-samples t test was used to evaluate the treatment changes in each group. Differences with probability less than 5% (P<0.05) were considered statistically significance.
The mean retraction Period was (4.1 months) in group1 and (3.8months) for group 2. Comparison of pretreatment and post treatment cephalometric evaluations in (G1) showed that the overjet was significantly improved. The mesiodistal position of the maxillary molars showed a small change (+0.53mm). Comparison of pretreatment and post treatment evaluations in (G2) showed that the incisors were significantly retracted. The maxillary molars were moved mesially (+1.5mm) (Table 1).
|
Group1 |
Groups 2 |
||||||||
T1 |
T2 |
P value |
T1 |
T2 |
P value |
|||||
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|||
Cephalometric Values |
|
|
|
|
|
|
|
|
|
|
SNA |
83.13 |
4.09 |
78.81 |
3.94 |
0.000** |
81.63 |
3.74 |
78.63 |
3.71 |
0.000** |
SNB |
76.25 |
4.06 |
76.25 |
4.06 |
- |
74.63 |
3.42 |
74.63 |
3.42 |
- |
ANB |
6.88 |
1.13 |
2.56 |
1.15 |
0.000** |
7 |
1.6 |
4 |
1.67 |
0.000** |
SN/MP |
32.88 |
3.52 |
32.69 |
3.58 |
0.197 |
36.88 |
8.22 |
37.19 |
7.8 |
0.544 |
U1/SN |
107.75 |
5.57 |
100.13 |
6.4 |
0.004** |
101.75 |
4.62 |
96.44 |
5.18 |
0.037* |
L1/MP |
97.25 |
4.86 |
96.56 |
2.38 |
0.587 |
94 |
4.87 |
95.44 |
3.83 |
0.016* |
U1/L1 |
119.75 |
7.07 |
127.75 |
7.72 |
0.004** |
124 |
3.3 |
128.75 |
6.16 |
0.031* |
U6/SN |
74.75 |
4.17 |
74.56 |
5.3 |
0.822 |
74.13 |
3.56 |
75.88 |
3.51 |
0.000** |
Linear (mm) |
|
|
|
|
|
|
|
|
|
|
U6M-PTV |
28.56 |
1.29 |
29.09 |
1.31 |
0.000** |
27.31 |
4.04 |
28.81 |
3.52 |
0.001** |
Overjet |
9.63 |
1.85 |
2.69 |
0.46 |
0.000** |
7.56 |
1.08 |
2.25 |
0.38 |
0.000** |
Soft Tissue Values Angle(o) |
|
|
|
|
|
|
|
|
|
|
Nasolabial Angle |
105.25 |
10.78 |
111.63 |
13.24 |
0.003** |
112 |
15.6 |
113.75 |
14.41 |
0.155 |
Inferior Labial Sulcus Angle |
123.13 |
3.87 |
126.88 |
4.73 |
0.003** |
121.38 |
4.37 |
123.75 |
3.33 |
0.342 |
Linear (mm) |
|
|
|
|
|
|
|
|
|
|
E-UL |
-1.56 |
2.56 |
-3.31 |
1.39 |
0.029* |
-2.25 |
2.12 |
-3.06 |
1.02 |
0.122 |
E-LL |
-0.06 |
1.82 |
-1.81 |
1.19 |
0.024* |
-0.25 |
2.25 |
-0.75 |
1.49 |
0.502 |
Table 1 Comparison of pretreatment (T1) and post treatment (T2) measurements
*P <0.05; **P <0.001
There was no significant difference in reduction of overjet between the two groups. They were both effective in treating excessive overjet, with approximately 5mm decrease (Table 2). However there was a significance difference in the reduction of SNA angle (-4.31o in G1 and -3o in G2). Comparisons of the soft-tissue measurements between T1 and T2 showed that the soft tissue profile was improved in both groups (Figure 4).
|
Variable |
Group1 |
Groups 2 |
P Value |
||
|
Mean |
SD |
Mean |
SD |
||
|
Cephalometric Values |
|
|
|
|
|
|
SNA |
-4.31 |
0.37 |
-3 |
0.27 |
0.000** |
|
SNB |
0 |
0 |
0 |
0 |
- |
|
ANB |
-4.31 |
0.37 |
-3 |
0.27 |
0.000** |
|
SN/MP |
-0.19 |
0.37 |
0.31 |
1.39 |
0.341 |
|
U1/SN |
-7.63 |
5.15 |
-5.31 |
5.84 |
0.415 |
|
L1/MP |
-0.69 |
3.41 |
1.44 |
1.29 |
0.122 |
|
U1/L1 |
8 |
5.37 |
4.75 |
5.01 |
0.231 |
|
U6/SN |
-0.19 |
2.27 |
1.75 |
0.38 |
0.032* |
|
Linear (mm) |
|||||
|
U6M-PTV |
0.53 |
0.17 |
1.5 |
0.76 |
0.003* |
|
Overjet |
-6.94 |
1.52 |
-5.31 |
0.92 |
0.022* |
|
Soft Tissue Values |
|
|
|
|
|
|
Nasolabial angle |
6.38 |
3.96 |
1.75 |
3.11 |
0.021 |
|
Inferior Labial Sulcus Angle |
3.75 |
2.31 |
2.38 |
6.59 |
0.586 |
|
Linear (mm) |
|||||
|
E-UL |
-1.75 |
1.81 |
-0.81 |
1.31 |
0.255 |
|
E-LL |
-1.75 |
1.73 |
-0.5 |
2 |
0.203 |
Table 2 Comparison of pretreatment and post treatment changes (T2-T1) between groups
*P < 0.05; **P < 0.01
A primary concern in orthodontics has been the development of techniques to adequately preserve anchorage.15,16 The inclusion of the second molar is a simple to enhance anchorage in day to day orthodontic practice. It is simple and cost effective in public health care delivery system as it does not require any extra armamentarium or clinical training.
Many studies showed that inclusion of the second molar might not be an effective method for anchorage preservation during en-masse anterior segment retraction in treating class ІІ malocclusions.17–20 In the current study, after treatment with premolar extraction and combining it with alveolar corticotomy, the maxillary incisors were significantly retracted and both groups had proper overjet. These results suggested that both methods were useful to improve maxillary dental protrusion and inter incisal relationships.
The horizontal movements of the upper first molars were statistically significant in both groups. Difference was (0.53mm in group1 and 1.5mm in group2). From a clinical point of view, this difference is clinically insignificance, because in group2 (1.5mm) mesial movement of the upper first molar accompanied by mesial crown tipping of 1.75o, does not clinically affect the treatment result.
According to Nanda, we can classify the anchorage in our study as type A anchorage. This category describes the critical maintenance of the posterior tooth position. Seventy-five percent or more of the extraction space is needed for anterior retraction.21
In previous reports, treatment of premolar extraction patients with traditional mechanics, the maxillary molars were usually mesialized approximately 30% in to the extraction space with excellent cooperation for maximum anchorage.4,17,18 The variation in upper molars mesial movement between the current study and the studies reported is due the alveolar corticotomies.
Frost22 found a direct correlation between the severity of bone injury and the intensity of its healing response, which occurred mainly as a reorganized activity and accelerated bone turnover at the surgical site. This type of healing response was named "Regional Acceleratory Phenomenon" (RAP) and was defined as a temporary phenomenon of increased localized remodeling to rebuild the surgical site.23 Wilcko24,25 noticed that the reduced mineralization created by the corticotomies (osteopenia) of the alveolar bone housing the involved teeth and the subsequent RAP were the reasons behind the rapid tooth movement following corticotomies.
Closing spaces in posterior areas requires moving the teeth in the mesiodistal orientation of the alveolus.26 Have clearly shown that the insult of circumscribing corticotomy cuts alone will not produce an osseous response that is sustainable enough to permit movement of tooth roots through large amount of bone in the mesiodistal orientation of the alveolus.26 Tooth movement can only be sustained post-corticotomy surgery if a thin layer of bone is present over the root surface in the direction of the intended tooth movement.27 Additionally, continued tooth movement prevents tissues immediately adjacent to the root from remineralizing and that is reason why the reactivation was done every two weeks.
In the current study, accomplishing en masse retraction movement in the most efficient manner possible will require a considerable amount of alveolar preparation at the extraction site space. To provide for a very thin layer of bone over the entire length of the distal root surface of the canine requires ostectomy in the area previously occupied by the root of the first bicuspid, leaving a very thin layer of the of bone over the entire length of the distal canine root.
Orthopedic forces (450gr/side) were used because it is more efficient than orthodontic forces.27 The initiation of the space closure was delayed for two weeks to allow the thin layer of bone to demineralized. In opposition to "Periodontally Accelerated Osteogenic Orthodontics" (PAOO) technique, described by Wilcko,17 no bone grafting material was included in the treatment, because no sign of dehiscences or fenestrations over the roots of the anterior teeth was observed and the roots were not moved beyond their physiological borders.
Lee et al.28 & Sebaoun et al.29 reported systemic and histological evidence supporting the theory that the alveolar responses to corticotomy is localized in the injury site and doesn't extend to further teeth. Decreased cortical resistance and increased bone remodeling seem to allow safer and stable retraction of the anterior segment without overloading the posterior segment.
In current study, no significant reduction in the crest bone height, decrease of attached gingiva, marked apical root resorption, or devitalization were observed after the orthodontic treatment.
Alveolar corticotomies on the anterior teeth combined with inclusion of second molars proved to be efficient for intraoral anchorage reinforcements for en-masse retraction of the maxillary anterior teeth. It is hoped that more investigations with larger samples will be forthcoming to further evaluate this approach of treatment.
None.
The authors declare there are no conflicts of interest related to the article.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.