Journal of
eISSN: 2373-633X


Research Article Volume 1 Issue 3
British Columbia Institution of Technology, Canada
Correspondence: Virali Shah, Memorial-Sloan Kettering Cancer Center, 1275 York Ave, New York 10065, USA
Received: October 28, 2014 | Published: December 5, 2014
Citation: Shah V, Hernandez H, Ng I, et al. An investigation of factors influencing mammography screening participation in British Columbia. J Cancer Prev Curr Res. 2014;1(3):84-91. DOI: 10.15406/jcpcr.2014.01.00017
Breast cancer is the most common cancer among women. Mammography screening greatly reduce breast cancer mortality in women between the ages of 50 and 69. Despite the well publicized importance of attending mammography, screening rates in British Columbia (BC) continue to remain below an ideal 70% screening rate. This study examines the factors that influence mammography screening participation in women between the ages of 45 to 65, living in different regions of BC. Literature review has shown that age, ethnicity, socioeconomic status, obesity, smoking, urban and rural living, previous Pap smear screening, having a regular family doctor, and recent physician access affect screening attendance. Data from the 2006 Canadian National Census and the 2005 Canadian Community Health Survey was obtained in order to determine the influence of factors in regions of BC. Results showed that increasing obesity and low education were significantly correlated with lower mammography screening rates in BC, confirming previous literature trends. Older age was found to correlate with increased mammography screening attendance. Knowledge of factors that influence mammography screening in specific regions of BC can help provide region-specific recommendations and improve screening attendance, thereby increasing the likelihood of early detection and reducing breast cancer mortality.
Keywords: mammography screening, community health, screening
BC, British Columbia; MSP, medical services plan; SMPBC, screening mammography program of British Columbia; PHSA, provincial health services authority; Pap, papanicolaou; WHO, world health organization; BMI, body mass index; SES, socio economic status; CCHS, Canada community health survey; BCCA, British Columbia cancer agency
Breast cancer is the most common cancer diagnosis in Canadian women.1 Each year, more than 20,000 women are diagnosed with breast cancer and over 5,000 die from it.2 One in every nine women will be diagnosed with breast cancer over the course of their lives.1 A mammogram is a diagnostic tool that is used to detect breast cancer. It can identify cancers as early as stage I, less than 2 cm, which may not be detected during a clinical breast examination by a physician.3 Early breast cancer detection greatly contributes to improved prognosis and treatment outcome. It can reduce breast cancer mortality by 20-25% in women aged 50-69.4 Therefore, Canadian experts suggest that the benefits of screening outweigh the risks for women aged 50 to 69.2
The Screening Mammography Program of British Columbia (SMPBC) was established in 1988 by the British Columbia Cancer Agency (BCCA).2 The national mammography screening participation rate target is 70% for women aged 50 to 69.1 However, current mammography screening rates in British Columbia (BC) are falling short of the target despite the fact that the SMPBC has been running for the last 22 years and the cost of screening mammography is covered by the Medical Services Plan (MSP) of BC for women aged 50-69.2 The gap between the target and actual screening rates alludes to the existence of factors that negatively influence women’s decision to participate in the screening program. In order to reach the target of 70% mammography attendance and decrease the risk of breast cancer mortality, these factors must be identified so that appropriate countermeasures can be taken.
Many studies have investigated factors that influence women’s decision to participate in regular mammography screening. Most of these studies were conducted in the United States (US) and few were focused on Canada. The studies carried out in Canada focused on screening mammography participation in Ontario. The Provincial Health Services Authority (PHSA) in BC has recently published an in-depth investigation of the current state of mammography screening in the province.5 However, this publication does not address all the factors that have been identified in other comprehensive American and Canadian studies. In addition, PHSA divided health services in BC into 16 health service delivery areas, yet the report addressed mammography-screening issues for the entire province as a whole. The reality is that different factors are likely to predominate in different regions of BC; therefore, countermeasures would be more effective in improving screening rates if implemented in specific PHSA health service delivery area through their own resources.
The purpose of this study is to investigate factors that affect mammography screening attendance for asymptomatic women between the ages of 45 and 65 in different regions in BC, identify which factors are more predominant in specific regions, and suggest recommendations specific to the needs of each region in order to improve mammography screening attendance. These factors include age, ethnicity, obesity, smoking, socioeconomic status, population density, previous Papanicolaou (Pap) smear screening, having a regular family doctor, and recent physician access.
Literature review has unveiled various factors associated with mammography screening participation. These factors include age, ethnicity, obesity, smoking, socioeconomic status, urban and rural residency, previous Pap smear screening, having a regular family doctor, recent physician access, and other personal, interpersonal, and situational factors.
Age
Literature has reported that elderly women are less likely to participate in mammography screening6‒8 However, it has been difficult to establish what exactly constitutes “elderly” or “older age” because various studies have employed different age ranges. Studies from the US have used cut offs such as 65+ and 80+, whereas Canadian studies tend to be restricted to the 50-69 age range. Research shows that while physicians may play a greater role in older women’s mammography screening attendance, other factors such as media and available time may have a greater impact for younger women.9,10
Ethnicity
Literature has consistently reported an association between ethnicity and mammography screening participation.11,12 Studies show that first generation women of Hispanic, Chinese, Korean, Vietnamese, and Cambodian ethnic background have reduced participation in mammography screening.13 Muslim women, who generally originate from west Asian locales, tend not to attend mammography screening as frequently as non-Muslim.14
Obesity
Most studies have adopted the World Health Organization (WHO) classification of body mass index (BMI) as a measure of being overweight and obese. WHO defines the normal BMI range as between 18.5-24.0 kg/m2 and the range for being overweight 25.0-29.9 kg/m2; these are followed by Class I (30.0-34.9 kg/m2), Class II (35.0-39.9 kg/m2), and Class III (> 40 kg/m2) obesity.15 The majority of published studies found a statistically significant correlation between Class III obesity and decreased participation in mammography screening, where as correlations for other classes such as being overweight were not deemed statistically significant.16 Research also reported ethnic disparities among obese women, mainly between white and black women, due to different perceptions of the ideal body image.16
Smoking
Literature has consistently reported that women who smoke are less likely to participate in mammography screening compared to their non-smoking counterparts.11,17‒19 According to a previous study, even though both smokers and non-smokers are equally likely to receive a recommendation to attend screening by primary care physicians, smokers are less likely to follow through with the recommendation.11 Another study suggested that lower participation rates could be a result of smokers being primarily concerned with smoking cessation programs.19 These results allude to possible behavioural and attitudinal differences between smokers and non-smokers that can impact mammography screening attendance.
Socioeconomic Status (SES)
Various studies have reported a positive correlation between lower SES status and decreased participation in mammography screening.11,20‒21 One study found that women with higher education were more likely to go for their mammography screening when compared to less educated women.20 Other studies have looked at income levels and participation rates for mammograms and found that women with annual household income of < $15,000 were less likely to attend mammography screening in the past two years (2009-2011) when compared with women whose annual income was greater than $15,000.21
Urban vs. rural living
Literature reports that women who live in rural areas are more likely to attend their first mammography screening if they receive a physician referral, whereas urban women have a greater probability of attending a first mammography screen regardless of whether they received a physician referral or not.22 Rural women are also more likely to adhere to continued screening after the first visit while urban women tend to have a lower rate of return.22 One study investigated urban and rural living and SES and found that women who had low SES in urban areas were less likely to attend mammography screening and should be targeted to promote attendance.20
Previous pap smear screening
Literature has consistently found that women who have had a Pap smear test are three times more likely to participate in mammography screenin.12,18,23‒24
Having a regular family physician
Several studies have found that having a regular family physician is a strong predictor of attending mammography screening.11,18‒19,25‒26
Recent physician access
Physician access is a strong predictor of mammography screening attendance.11‒12,24,27 Some studies that identified having a family doctor as a predictor of mammography attendance found that this association was no longer significant if the patient had not had contact with the physician in the past 12 months. The study suggests that recent physician access is what impacts screening attendance.27
Other factors
Other personal, interpersonal, and situational factors have also been reported in the literature; however, there have been no extensive research on each of these factors to confirm the initial findings. Personal factors include family history of breast cancer, individual health status, physical activity, marital status, and psychological factors.12,28 Interpersonal factors refer to those related to other people, such as healthcare provider support and support from one’s social network.12 Situational factors refer to environmental factors such as health service availability and effect of messages from the media.12
An initial search was conducted for factors that influence mammography-screening participation in North America. This online website search was carried out through the EBSCO, PubMed, Medline, Ovid, and CINAHL databases. The search was limited to articles in English that were published in Canada or the US in order to eliminate social differences as confounding variables. Recent studies from 2005 to 2010 were used in order to ensure that findings would be as up to date as possible. Type of articles included cross-sectional studies, experimental studies, case studies, reviews, and expert opinion on the subject. Words used in the search included “mammography”, “breast cancer screening”, “breast cancer prevention”, “screening compliance”, “screening adherence”, “mammography participation”, “mammography attendance”, “British Columbia”, “Canada”, and “United States.”
A preliminary list of factors that influence mammography screening was compiled mainly from two review articles, both of which were specific to Canada and were published in 2009, in combination with other factor-specific research articles. One additional review article that was published in the US was also employed to validate factors influencing mammography screening in Canada.
Factors were then narrowed down to: age, ethnicity, overweight or obesity, smoking, SES, recent Pap smear screening, having a regular family physician, and recent physician access. Personal factors (breast cancer and/or mammography screening knowledge, fear or anxiety, lack of time), interpersonal barriers (health care practitioner and social network support), and situational factors (health services deficiencies and effect from the media) were eliminated from the investigation due to the lack of data availability from statistical resources.
Data collection
A minimum of 3 articles and a maximum of 5 were obtained to support each factor, using the same databases as in the initial search. Criteria for the sample or population in the publications were: female, aged 40 to 79, asymptomatic, no personal history of breast cancer, no breast implants, resident of Canada or US (or both), born in North America or a first generation immigrant in North America. The age range of 40-79 was chosen because this was the most common age range in published studies. The publication date range from 1998 to 2010 was chosen to accommodate the fact that studies for some factors (for example obesity) had been conducted prior to the 2005 cut off, and once studies on one factor had been done, peer-reviewed, and published, they were likely not repeated to avoid redundancy unless a significant change had occurred in the study.
Older age was defined as being 65 years and older because this was suggested from literature and also because this was in concordance with the age range. SES was analysed in terms of education and income because both were measurable components that ultimately contributed to one’s socioeconomic status. Low education was defined as those who had less than a high school certificate or equivalent as investigated in the national census conducted by Statistics Canada, and low income was as defined by Statistics Canada. Previous Pap smear screening was defined as having a Pap smear in the previous three years and recent physician access was defined as having accessed a physician in the last 12 months because both have been consistently utilized across literature to delineate each factor.
Mammography screening rates for women aged 50-69 were obtained from the Statistics Canada website. The 50-69 age range was chosen because this was the age range that received coverage for mammography screening under current provincial guidelines, in Canada. Data for examined factors were obtained from the 2006 Canadian National Census or the 2005 Canada Community Health Survey (CCHS), both retrieved from the Statistics Canada website. Data for all factors were not available from a one single publication, such as Statistics Canada or other resources. The 2006 Census was the latest dataset available; the next cycle of national census will be in 2011. The 2005 CCHS was chosen because it was the closest to 2006. The age range for all the data was 45-64 instead of 50-69 due to access limitations. Data for older age, low education, low income, and ethnicity were obtained from the 2006 Census. Data for Pap smear screening, the proportion of women in BC who had a regular family physician, recent physician access, and the proportion of overweight or obese women in BC were obtained from the 2005 CCHS. Data for smoking was obtained from the BC Statistics website because it was not available from Statistics Canada. It included both male and female and spanned across all age groups, as it could neither be extracted by gender nor by age groups.
Only the first generation of ethnic group data was collected because cultural effects on mammography screening attendance are likely to be the most pronounced in this group as compared to subsequent generations. The division of different ethnic groups is taken from the 2006 Canadian Census. “Latin Central and South American” subgroup consists of people of Hispanic origin. “West Asian regions” refers to countries such as Afghanistan and Iran. “West Asians” refer to the Muslim ethnic group. “South Asians” consist of ethnic groups from Bangladesh, India, and Sri Lanka. “East and Southeast Asians” refer to people from countries such as Cambodia, China, Philippines, Korea, Japan, Thailand. “European” group includes those of Austrian, German, and Swiss origins. “British Isles” includes those of English, Scottish, and Welsh backgrounds. The “June 2005 boundaries” was selected for mammography screening rates, previous Pap smear screening, having a regular family physician, and recent physician access instead of the “2007 boundaries” because there was limited data for factors being investigated that were from 2007 and onwards, and 2005 was the closest year to 2006.
Below is a figure that shows the regional division of BC. A unique regional division of BC was created for this investigation because each of the statistical resources (SMPBC, Statistics Canada, and BC Statistics) used a different division system. For example, data retrieved from Statistics Canada were subdivided according to the June 2005 boundaries of health service delivery areas in BC, whereas the SMPBC used 5 regions as defined by the BCCA. The new regional map of BC for the purpose of this study was generated by amalgamating the regional division maps used by SMP, Statistics Canada, and BC Statistics (Figure 1).
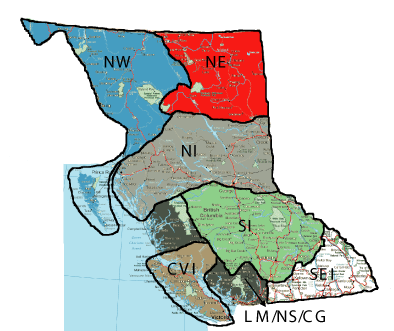
Figure 1 Regional Division of BC. The region located in the top left corner is the Northwest region (NW), the region to its right is the Northeast region (NE). The section below the above two regions is the Northern Interior region (NI). The region below NI the Southern Interior region (SI), Coastal Vancouver Island Regions (CVI) is the region that includes all of Vancouver island and a small portion off of the island along the coast. Southeast interior (SEI) is the region that is in the far right of the map. Lower Mainland/Northshore/Coastal Garibaldi (LM/NS/CG) is the region that includes lower mainland and a small region along Garibaldi.
Data analysis
Weighted averaging based on population size was done for mammography screening rates as well as data for all the factors in order to minimize possible skewing effects due to the area of each region. Trends in the effect of factors on mammography screening rates were assessed for significance through hypothesis testing.
As seen in Table 1, the prevalence of each of the factors affecting mammography screening varies greatly value showing level of significance among the different regions of BC. The northern regions of BC have the greatest proportion of overweight women compared to the rest of the province with the NW topping out at 50% of the study population. Only the LM/NS/CG region is considered an urban area, with a population density greater than 400 persons per km2, while the rest of the province is rural. The NI has the greatest proportion of women who are smokers at 25%, followed closely by the NE and SI regions (23% and 22%). The lowest proportion of smokers is found in the LM/NS/CG region at 15% of the study population. Taking age into consideration, more women living in the SEI (40%), CVI (38%), and LM/NS/CG (34%) fall into the 65 years and over age range when compared to the rest of the province. SES can be measured partially by income and education. Although the percentage of the low income population is small throughout the province, averaging at 8.8%, the LM/NS/CG region stands out at 14%, followed by the NW region at 10%. The NI (18%) and SI (17%) regions of BC have the greatest percentage of the study population that has a low education, which is considered education less than a high school diploma, with the NW coming out on top at 27%. A high percentage of the population in all of the regions of BC appears to have recent physician access (87% overall) within the last 12 months and a regular family physician (94% overall). Only the NE region has a significantly lower percentage of the population with recent physician access (73%) and with a regular family physician (88%). The average percentage of the population across the province that attended a Pap smear screen within the last 3 years was 69%. The NW (81%) and CVI (78%) regions stand out as have a higher than average attendance to Pap smear screening whiles the NE region is significantly lower in Pap smear screening participation at 54%.
BC Region |
Factors Influencing Mammography Attendance |
|||||||||
Over weight |
Population Density |
Smoking |
More than 65 y. o. |
Socioeconomic Status |
Regular Physician Access |
Regular Family Dr. |
Regular Pap Test |
|||
Category |
Density(Persons/Km2) |
Low Income |
Low Education |
|||||||
Northwest |
50% |
Rural |
0.6 |
21% |
26% |
10% |
27% |
94% |
95% |
81% |
Northeast |
40% |
Rural |
0.5 |
23% |
20% |
5% |
21% |
73% |
88% |
54% |
Northern Interior |
42% |
Rural |
1.4 |
25% |
26% |
8% |
18% |
88% |
96% |
69% |
Southern Interior |
33% |
Rural |
1.3 |
22% |
33% |
8% |
17% |
86% |
96% |
68% |
Southeast Interior |
27% |
Rural |
22.4 |
17% |
40% |
8% |
14% |
89% |
97% |
64% |
LM/NS/CG |
26% |
Urban |
638.2 |
15% |
34% |
14% |
14% |
88% |
93% |
67% |
Coastal Van. Island |
38% |
Rural |
87.8 |
17% |
38% |
8% |
12% |
88% |
95% |
78% |
Table 1 Summary of mammography screening factor prevalence among the BC regions as a percentage of the study population of females aged 45 to 65 years
Scatter plots (Figure 2) show how mammography screening rates vary with prevalence of factors, the data showed that only overweight BMI (t = 2.705, tcrit = 2.571, α = 0.05), low education (t = 4.909, tcrit = 2.571, α = 0.05), and age greater than 65 (t = 3.747, tcrit = 2.571, α = 0.05) had significant correlation across the province of BC. Increasing proportion of the population with an overweight BMI or low education appeared to have a negative influence on mammography screening participation. The opposite trend can be said for age greater than 65 where increasing proportions of the population that fall within this category show increasing attendance to regular mammography screening. None of the other factors that were investigated in this study appear to have a significant effect throughout all regions of BC.
The aim of this study was to investigate factors influencing mammography screening attendance rates in different regions of BC. Based on literature review, different factors such as age, ethnicity, obesity, smoking, SES, urban/rural, previous pap screening, regular family physician, and recent physician access had different impact on women’s decision for participation in screening. Results indicate that each of these factor investigated had varying influence on mammography screening behavior in different regions of BC.
Age
One study found that women 65 years of age or older are less likely to attend mammography screening compared to younger women, as older women may be “less concerned” about mammography screening due to lack of symptoms and knowledge about age as a risk factor for breast cancer.6 Older women are more likely to attend screening if it was recommended by their doctor; they seem to prefer a doctor’s recommendation over media, family, or friends.7 In BC, the SI and CVI regions have the highest percentage of population as being over the age of 65 (40% and 38%), followed by the LM/NS/CG and SI regions (34% and 33%). These 4 regions also have the highest mammography screening rates in BC. The discrepancy between results from this study and findings from the literature may be explained by the notion that if older women visited their doctors more regularly than younger women, then they are more likely to be referred for mammography screening. One study suggests that the role of the media and changing relationships between husband, children and friends may be a determinant factor in lower adherence rates in aging women.9
Ethnicity
Previous research found that one of the reasons for ethnic women to have decreased participation in mammography screening is language barriers, speaking English, and illiteracy in mother tongue (Unable to read or write in the a language) or English.29 Chinese American women may not participate in mammography screening due to knowledge, attitudinal behaviors, Eastern cultural views, and individual perception of risk Wang et al.13 developed the Chinese culture scale to evaluate “Eastern cultural views.”.30 Another study looked at various Southeast Asian groups, and found that Chinese and Korean women are more likely to go for mammograms compared to other Southeast Asians. Women of Cambodian origin are the least likely to go for mammograms (78.52%) compared to Korean women (30.23%) or Chinese women (20.10%).13 When they looked at subsequent mammograms within 10 months, again Cambodian women fell at the lowest rank (11.41%) compared to Chinese women (57.63%) who are more likely to go for subsequent mammograms. This is a significant statistic as in British Columbia there is population from each of these countries. However these rates are still quite low when compared to Caucasian women residing in BC.31 Some of the possible reasons for these results are age, years lived in USA, education level, employment status, annual household income, health insurance, language, concordant physician, and viewing media negatively.13 Another study shows that Muslim women tend not to go for mammography screening because of discomfort, embarrassment, belief that there is no cure for breast cancer, and the perception that mammograms are a health hazard rather than a useful detecting tool.14 The LM/NS/CG region is the most ethnically diverse region in BC. Among the ethnic minority groups within this region, a majority of the population is from East Asia. The rest of the BC regions have a majority of the population from British Isles and Europe. Ethnic background does not show statistically significant correlation with mammography screening rates in BC so this factor likely does not strongly influence mammography-screening participation.
Obesity
Obese women tend to have lower adherence to mammography screening.32 In BC, the NW, NI, and NE regions have the highest proportion of overweight persons (50%, 42%, 40%), as well as the lowest screening rates in BC (37%, 43%, 43%). There is a significant correlation between being overweight and decreased mammography screening participation in BC, as shown in (Figure 2). One review suggested that obese women may delay breast exams because of poor self-esteem, poor perceived body image, and embarrassment.16 Another study found that obese women perceive a lack of respect by healthcare practitioners and often avoid screening to avoid unsolicited weight loss advice.15 Obese women may have a negative attitude towards screening and increased anxiety related to loss of physical privacy prior to screening.33 A survey of potential barriers to mammography screening among overweight or obese women found that pain and discomfort were the most common factors.33 Knowledge about the physical aspect of the procedure and how it can be influenced by having proportionally larger breasts may heighten the fear of pain. Furthermore, obese women may postpone screening because they are more likely to have chronic conditions, which take priority in their healthcare.34
Smoking
Poole et al found that smoking is correlated with decreased mammography screening.18 In BC, the NI, NE, SI, and NW regions have the highest proportion of population who smoke (25%, 23%, 22%, 21% respectively). The mammography screening rates for these 4 regions are the lowest in BC, except for the SI. However, the correlation between proportion of smokers and mammography screening rates is not statistically significant across the province of BC. The lower rates in the 4 regions mentioned previously may suggest that smoking is associated with lower screening rates in these regions of BC but can also be due to a combination of factors since the study in this data cannot be extrapolated to come to this conclusion. Interestingly, one study found that the majority of women who smoke are knowledgeable about smoking as a risk factor to breast cancer; however, lower mammography rates still exist.17 One review suggested that female smokers who are unwilling or unable to quit are less concerned about health promoting factors such as mammography screening.11 Another study argued that these women may have an overall negative attitude towards health and a lower level of perceived benefit compared to non-smokers.18 Other studies claim that part of the reason for lower participation rates could be due to the fact that female smokers’ first concern may be smoking cessation programs.19 It is plausible that lower screening rates may be merely a result of the shifting of time and energy towards trying to quit smoking.
SES
In BC, the greatest proportion of the population that had low income was found in the NW and the LM/NS/CG regions compared to the rest of BC. The highest proportion of low education in the regions of BC is found in the NW and NE regions. While low education is correlated with decreased mammography screening attendance, low income, on other hand, seems not to have any effect on screening rates (Figure 2). Thus, low education as a measure of low SES does appear to influence mammography-screening participation in BC, confirming the trend outlined in literature. SES is not only affected by urban/rural factor but may also be influenced by other factors. A study suggests that people who fall under the low SES category have lower levels of emotional support, breast cancer education and social interactions.35‒36 Other research indicates that people with low SES also have greater commitments, as they may have higher number of dependents and greater workload and responsibilities.35 These women may not view screening as a priority in their lives. In terms of income, health insurance does not appear to be a barrier for women living in Canada since the cost of screening mammograms are covered by the health care system. Other research has supported the fact that if women who were under low income received more emotional support as opposed to tangible support, they were more likely to participate in mammography screening.36 Suggestions made by previous research include providing more education to low SES groups to encourage mammography screening participation.37 Education can be either about mammography screening or career development or both.
Urban vs. rural living
Research indicates that urban women are more likely to attend their first mammography screening compared with rural women.22 Some of the influencing factors for this include exposure to media and testing center accessibility. Unfortunately, urban women tend not to continue with their subsequent mammography tests.22 Reasons for this may include a busy lifestyle, which may interfere with their mammography attendance.
The rate for the first screening for rural women is lower than urban women; however, consecutive mammography screening rates is higher amongst rural women when compared to urban women.20 This may be due to a less busy lifestyle for rural women. Research found that rural women tend to go to their first mammography screening after physician recommendation. They also proposed that lack of cancer education, accessibility, and inconvenience may be factors to play a role in this.38
One study investigated SES in urban and rural areas.20 It found that higher SES status was associated with continuing mammography participation in urban areas but had no effect on rural areas. They also found lower screening rates in urban areas compared to rural areas, but this difference in participation rates decreases with an increase in SES.
The LM/NS/CG is the only region that can classified as an urban region in BC. The rest of the BC region falls under rural. This study does not show significant correlation between population density and mammography screening attendance in BC. Other factors are likely to have greater impact.
Previous pap smear screening
A number of studies and reviews have found a positive association between previous Pap smear screening and mammography screening attendance.12,18,23‒24 One study suggested that women who had previous Pap smear screening are already knowledgeable about preventative programs and services, and they may have overcome barriers associated with screening.24 In BC, screening rates for most regions are around 50% for mammography and well above 60% for Pap smear. This is opposite of what has been suggested in the literature. One possible explanation is that Pap smear screening can be carried out by physicians as well as nurses whether it’s in a private clinic or at a community health centre, whereas women can only obtain a screening mammogram at BCCA centres or through its mobile van service. There is no significant correlation in this study between Pap smear screening history and mammography screening participation in BC.
Having a regular family physician
Several studies have found a regular family physicians to be positive predictor of mammography screening attendance.11,18‒19,25‒26 Not only is screening attendance higher for women who have regular family doctors compared to those who don’t have family doctors, but only have a usual source of care such as a walk-in clinic.11,39 This suggests that health-care relationships do impact on the utilization of screening services.39‒40 The positive client-health care provider relationship could mean that women who have regular family doctors are more likely to trust their health care providers and adhere to their advice. Findings from this study indicate that the majority of women between the ages of 45-64 in BC have a regular family physician. The NE region has the lowest proportion (88%), while the SEI, SI, and NI regions have the highest percentages (97%, 96%, 96%). Despite these results, mammography screening attendance province-wide remains below the goal of 70%. In this study, here is no statistically significant correlation between having a regular family physician and mammography screening participation in BC. Results indicate that having a regular family doctor may not be a strong predictor for attending mammography screening in BC.
Recent physician access
Recent physician access has been positively associated with mammography screening attendance.11,27,41 Women who have had contact with a medical doctor within the last 12 months are more likely to have accessed mammography screening in the past 2 years compared to those who have not.11,18 A possible explanation could be that women who have had recent contact with a doctor are more likely to get a physician recommendation for mammography screening. Data on the frequency of physician recommendations were not available for this study. In BC, despite the high percentage of women who have a regular family doctor, the proportion of women between the ages of 45-64 who have had contact with a medical doctor within the past 12 months are generally lower. Interestingly, the NW region, which has one of the higher proportions of women between the ages of 45-64 to have a regular family doctor (95%), has the highest proportion of women who have had contact with a medical doctor within the past 12 months (94%), but yet has the lowest mammography screening attendance in BC. There is no statistically significant correlation in this study between having recent physician access and mammography screening attendance in BC. This suggests that there are most likely other factors that have a higher impact in screening mammography attendance. Future directions might include research into the effect of physician recommendation frequency on mammography screening attendance.
Other factors
Literature review showed that other factors affect adherence to screening. In general, most women fear the lack of personal control in conjunction with becoming diagnosed with breast cancer.6 One study found that marital status affected mammography screening while another looked at hormonal replacement therapy as a promoter to screening.8,12 A further analysis is necessary to fully assess the true impact of these factors on the participation rates.
Limitations
This study had several limitations. Not all data were available from a single resource; therefore assumptions were made to account for any discrepancies this may have created. Assumptions that were made include an insignificant change in the study population between the years of 2005 and 2006, a good response to the surveys from which we extracted data, accurate self-reports of BMI, no interaction between the factors, and normal distribution of data. In reality, factors are likely to interact or could have a synergistic effect on mammography screening rates, and the degree of complexity of such interactions makes it more difficult to separate effect on screening rates due to one single factor. It is known that data are not normally distributed for some factors, namely the Pap screening and physician data, but the distribution information was not available for these and other factors; therefore the assumption of a normal distribution was made. Data availability may also have affected results. Data for smoking included both males and females and of all ages because it was not available specific to this study’s cohort of females, aged 45-65 years. The proportion of smokers was then assumed to be constant among all age groups and for both genders. An economic family was interpreted as consisting of a heterosexual couples or a single female parent family. It is possible that an economic family could be made up of a homosexual couples or a single male parent family; however, we were unable to account for these possibilities without omission of critical data. Depending on the particular region of BC, the ethnic composition within the study population was extrapolated for 3% to 48% (median of 29%) of the population for which we were unable to obtain pertinent data. Ethnic population data was sparsest among the regions of the northeast, southern interior, and southeast interior.
This study investigated factors influencing mammography-screening participation in regions of BC in asymptomatic women between the ages of 45 and 65. Specific factors examined were older age, ethnicity, SES, obesity, smoking, previous Pap smear screening, regular family doctor, and recent physician access. The regions in BC were CVI, LM/NS/CG, SEI, SI, NI, NE, and NW. Obesity, lower education, and smoking were the most prevalent factors in the NW region. In the NE, lower mammography screening may be influenced by a greater population that doesn’t have a regular family doctor, recent physician access, previous Pap smear screening, smoking, and obesity. Negative impact on mammography screening in the NI region may be attributed to higher smoking and obesity rates, older age, and low previous Pap smear screening attendance. Smoking and age appear to influence adherence to mammography screening attendance in the SI region. Older age and low Pap smear screening participation seem to affect attendance in the Southeast Interior region. Mammography screening attendance in the LM/NS/CG region may be associated with lower income, older age and low Pap smear participation. Older age, obesity, and smoking appear to affect mammography-screening participation in the CVI region. Women residing in an urban region do not seem to impact mammography screening for women being screened for the first time. However, literature suggests that women living in rural areas of BC may tend to adhere regularly to screening recommendation after their first mammography screening.
A secondary goal of this research is to provide possible recommendations specific to factors. This study is important because insight gained from knowledge can be used to promote mammography screening in BC and reduce risk of breast cancer. BC is an ethnically diverse province, so mammography-screening programs should be promoted in multiple languages and concordant to cultural norms. Physicians should be encouraged to play a more active role in initiating dialogue, sending out personal invitations, and recommending mammography screening. Topical analgesics such as 4% lidocaine gel applied to the skin and chest wall can be used to lessen discomfort during screening.42 However, the efficacy of this procedure may provide further research in terms of complexity and time required for pre-screening preparation. In 2010, the PHSA released the new “Breast Health Action Plan,” in order to provide equal opportunity for mammography screening to women in BC.5 This includes updating marketing material and translating them into different languages, introducing new routes for mobile screening vans, implementing local advocate programs and initiating collaborative community initiatives. Whether changes by the PHSA lead to improvements in mammography screening remains to be seen, however; a longitudinal study can provide insight of the effectiveness of recommendations. Lastly, future studies can be conducted in order to compare the results of this study, investigate factors that have not been addressed, and evaluate the effectiveness of proposed recommendations.
None.
Authors declare there are no conflicts of interest.

©2014 Shah, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.