Journal of
eISSN: 2373-4396


The presented case conveys two significant clinical messages. Firstly, the embolic risk for patients with non-compacted myocardium is high and anticoagulants should be prescribed in case of left ventricular dysfunction or atrial fibrillation even if the CHA2DS2-VASc score is low. Secondly, the presence of ventricular arrhythmias in a patient with congenital heart disease and preserved biventricular function should lead to search for other causes of enhanced arrhythmic substrate, such as non-compacted myocardium.
Keywords: Non-compacted myocardium; Ventricular arrhythmias
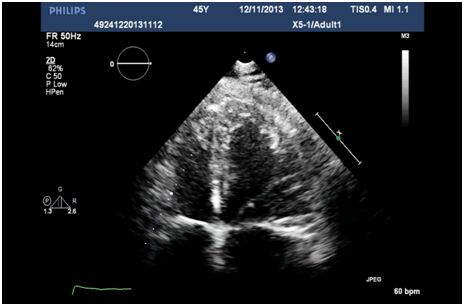
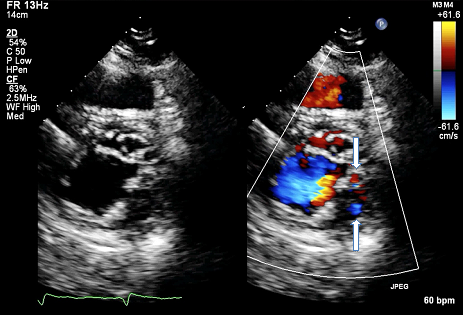
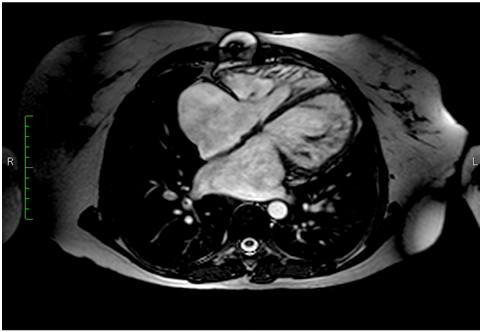
A 41 year-old-woman was admitted to our hospital for symptomatic complete atrioventricular block and atrial fibrillation. The patient had previously been diagnosed during childhood with partial atrioventricular septal defect and pulmonary valve stenosis; she had undergone at age 19 patch closure of primum ASD, repair of the left atrioventricular valve and open pulmonary valvotomy. She had a history of embolism in her right popliteal artery 10 years before admission for which she has been treated with oral anticoagulation. At admission, blood analyses including electrolytes were normal. Transthoracic echocardiography revealed a normal-sized left ventricle with good systolic function, increased left ventricular wall thickness and typical prominent trabeculations and intertrabecular recesses in the mid and apical segments of lateral and inferior wall pathognomonic for non-compacted myocardium (Figure 1A). Color Doppler imaging of the loosened myocardium demonstrated blood flow throughout the trabeculations (Figure 1B). Right ventricle was also mildly trabeculated with normal dimensions and preserved systolic function. There was no residual atrial shunt and there was mild left atrioventricular valve regurgitation and mild pulmonary valve stenosis. Cardiac MRI confirmed the diagnosis of left ventricular non-compaction with preserved left ventricular function, but also demonstrated the significant involvement of right ventricular myocardium (Figure 2).
A 24-hour Holter monitoring performed 3 months before admission documented episodes of non-sustained ventricular tachycardia and, therefore, she underwent an electrophysiological study before the implantation of a cardioverter-defibrillator (ICD). A ventricular tachycardia followed by ventricular fibrillation was induced and an ICD was implanted. Two years after ICD implantation the patient experienced an episode of sustained ventricular tachycardia converted with antitachycardia pacing (Figure 3). Noncompaction of the left ventricular myocardium is a rare condition thought to be determined by intrauterine arrest of compaction of the loose interwoven meshwork that gives rise to the fetal myocardial fibers [1]. The disease uniformly affects the left ventricle, but biventricular involvement has frequently been reported. Noncompaction of the left ventricle has been described as an isolated cardiomyopathy but may also be encountered in association with other abnormalities, such as congenital heart disease and neuromuscular disease [2]. Left or right ventricular outflow tract obstruction, atrioventricular valve abnormalities and conotruncal lesions are the most common congenital heart lesions that are associated with non-compacted myocardium [3]. The main clinical manifestations of non-compacted myocardium are arrhythmias, heart failure due to left ventricular systolic dysfunction and embolism [3,4]. Management of these patients should be tailored based on these complications.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.