International Journal of
eISSN: 2574-9889


Case Report Volume 2 Issue 6
1Weill Cornell Medicine Qatar, Medical Education, Qatar
2Feto Maternal Medical Center, Qatar
Correspondence: Badreldeen Ahmed, Professor of obstetrics Weill Cornell Medical College, Director of Feto Maternal Centre, 380 Al Markhiya St. P.O. Box 34181, Doha, Qatar, Tel 00 974 44756369
Received: August 30, 2017 | Published: October 11, 2017
Citation: Al-Abdulmalek1 A, Al-Thani A, Ahmed B. Rare case of recurrent fetal familial uretrocele. Int J Pregn & Chi Birth. 2017;2(6):174-177. DOI: 10.15406/ipcb.2017.02.00043
We presented a rare case of familial recurrent Ureterocle and duplex right kidney. The diagnosis was made at the anomaly scan at 19weeks. Our patient is a case of first-degree consanguineous marriage with multiple miscarriages, two daughters with congenital ureteroceles and one healthy boy. Postnatal ultrasound confirmed the diagnosis. In spite of prophylactic antibiotics the patient developed severe urinary tract infection. Voiding cysterourethrogram (VCUG) revealed aureterocele without vesicoureteric reflux. The urinary tract infection was recurrent and severe and required urgent cystoscopy and puncture of ureterocle.
Keywords: uretrocele, prenatal, ultrasound, genetics
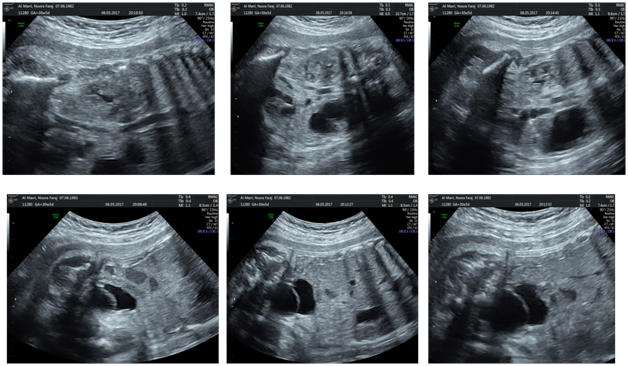
Mrs. N A is a 35 year-old patient, multigravida. She was seen at the Fetomaternal Clinic for follow up of her pregnancy. She is married to her first-degree cousin. A prenatal ultrasound performed in the prior visit revealed a single viable female fetus. The follow up ultrasound in the 19th week of gestation showed normal amniotic fluid volume and left-sided unilateral hydroneprosis with a full-distended bladder. Additionally, thinning out of the parenchyma and a dilated left ureter ending in a large left ureterocele. Douplex kidney was suspected. There was no any other abnormal scan findings. The patient was closely monitored. In the 22nd week of gestation an ultrasound scan showed left renal anterior posterior (AP) dilation, which measured 9 mm with normal kidney function indicated by normal liquor and a distended bladder. The dilatation increased to 18 mm in the 26th week seen by ultrasound scan, and no other abnormalities were noted (Figure 1). Subsequent antenatal and ultrasound were showed no marked changes in these findings.
Mrs. NA gave birth to a baby girl by cesarean section at 37 weeks of gestation because of oligohydramnios. The birth weight was 2.1 kg, had a measured length of 49 cm, (7th percentile) and a head circumference of 33 cm (<3rd percentile).
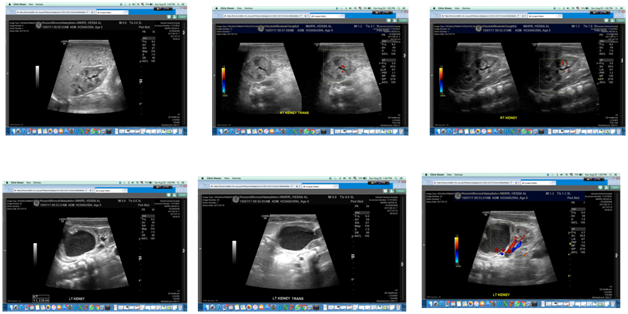
She did not require admission to NICU. Although the baby was started on prophylactic antibiotics (amoxicillin) since birth, on the 16th post-natal day, she was admitted to the emergency due to dysuria noticed by her mother. She was given the diagnosis of urinary tract infection (Klebsiella pneumoniae, sensitive to cefotaxime). Further workup was done when the patient was admitted to the hospital. Abdominal ultrasound (Figure 2) of the kidney revealed cystic area in the upper part of the left kidney, upper moiety, which is an indicative of duplex kidney. Urinary tract ultrasound showed a right kidney size of 4.4 cm and left kidney size of 6.8 cm by length and a left-sided duplex kidney with hydronephrotic upper motility. The scan also showed a tortuous dilated left ureter measuring 8.6 mm, 14.6 mm and 7.6 mm at the proximal, middle and distal regions respectively (Figure 3).
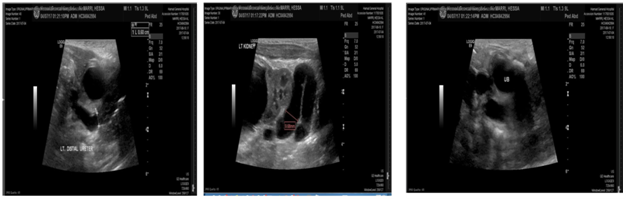
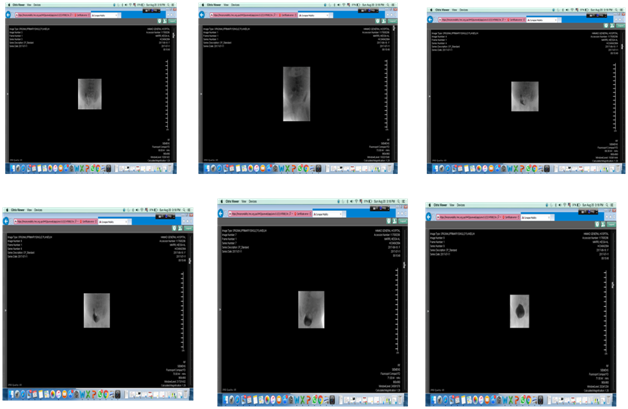
The young patient was booked for Voiding cysterourethrogram (VCUG), which was done uneventfully. VCUG revealed aureterocele without vesicoureteric reflux (Figure 4). Mrs NA 7 – years old daughter had a similar clinical condition at birth with left – sided ectopic duplex ureterocele, her condition was diagnosed only postnatally and corrected by surgery. Our young patient had the final diagnosis of a duplex right kidney and with large Ureterocle in the bladder. The patient is booked for cystoscopy and puncture of ureterocle. This was done laparoscopically and without any complications. The patient is undergoing further testing and genetic workup.
We have presented above a case of recurrent congenital Ureteroceles. One of the most common congenital anomalies is those which involve the kidney and urinary tract. Out of all prenatally detected congenital anomalies, approximately 20-30% of them involve the kidney or ureters.1 However, ureterocle is a rare congenital malformation defined as cystic dilatations of the terminal segment of the ureter that may occur in the bladder, urethra and in some cases both. The incidence of ureteroceles is approximately 1 in 500 being more common in Caucasian patients with predominance in female patients comparing with males with a ratio of 4-6:1. It is more common on the left side.2 Historically, the diagnosis was usually made after infants presented with urinary tract infection (UTI) as initial presentation to the healthcare setting. With current medical practice and technology and the advancement in equipment’s and training the diagnosis shifted to prenatal period. As a result, the early intervention (including prophylactic antibiotics) during childhood has improved the outcome and prognosis of this condition. According to the American Academy of Pediatrics, there are two classes of ureteroceles; the first case was intravesical being located in the bladder, and second is ectopic which is found at the bladder neck or in the urethra. An additional classification exists involving the single-vs-duplex categorization based on the number of collecting systems observed.3
Although ureteroceles commonly present as isolated cases, there have been several cases described which are familial similar to our case.4 This case illustrates the importance of prenatal diagnosis and postnatal work-up for ureterocele. With the development of ultrasound techniques there has been some movement towards prenatal diagnosis of conditions rather than waiting for the postnatal period. Early diagnosis and intervention improve the outcome of this condition. Prevention of progression may reduce the risk of life-threatening conditions or developing a chronic illness. A case described in 2015, highlights the importance of early intervention and prenatal diagnosis. An 18-year-old girl developed chronic renal failure due to bilateral ureteroceles which progressed over several years without any therapeutic intervention.5 Diagnosis of the ureterocele during the prenatal period would have likely prevented the irreversible structural and functional changes in the kidney.
Although renal development begins in approximately the 5th week of gestation, the kidneys are usually too small to be detected by ultrasound. This anomaly is usually diagnosed during the 2nd trimester scan.6 One of the common presentations of renal abnormalities is hydronephrosis which may be caused by several conditions including ureteropelvic junction obstruction, ureteroceles and many others. Our patient’s prenatal scan showed hydronephrosis, a left-sided renal AP dilation of 9mm and 18mm at 22 and 26weeks respectively, which are greater than the threshold during this period (20-30weeks, should be <8mm). (AH) Along with the AP dilatation, a white echogenic septum was seen in the bladder, which is most likely a ureterocele. The suspicion of ureterocele was confirmed by ultrasound in the postnatal period after the patient presented with symptoms suggestive of UTI. Ureteroceles may have a wide spectrum of presentations ranging from urinary tract infections to hematuria, abdominal pain, palpable mass, incontinence or failure to thrive in neonates.7 The results of the VCUG in our patient suggest that there is no vesicoureteral reflux which is commonly seen in patients diagnosed withureterocele. The presence of reflux has an impact on the treatment course and prognosis of the condition; therefore, VCUG should be part of the post-natal evaluation of ureteroceles.7
The pathogenesis of ureterocele is not well understood, but the most commonly accepted theory involves the Chwalla’s membrane, which fails to perforate during developmental stages. The incomplete breakdown of the ureteral membrane, between the ureteral bud and the mesonephric duct, will result in an obstruction. This thought to explain the formation of ureterocele.8 Another theory suggests failure to develop of musculature and dilation of the intramural ureter during embryological development of the bladder and trigone, which results in obstruction of the ureteral orifice leading to the ureterocele’s formation.8 Several molecular signaling pathways are involved in the process, and the risk of malformation may happen at any stage in pathway. Recent studies have found genetic influence on the maturation and development of the ureteral system and the kidneys. Genetic alternation in certain gen loci may lead to the development of familial pattern of ureteroceles.9
Sözübir et al.4 document the largest series of familial cases of ureteroceles, giving evidence for genetic background. They have reviewed retrospectively the charts of patients with familial ureteroceles seen between 1992 and 2002.4 This is the largest series of familial ureterocele patients in the literature. Three of the families have twin siblings with ureteroceles. Our patient is a recurrent case of ureterocle in a single pregnancy. The first familial case of twin siblings with ureterocele was reported in 1936 by L. W. Riba, which was simple systemureterocele in identical twins.10
We are reporting another case familial ureterocele, which is a rare. In this case of first-degree consanguineous marriage there were multiple miscarriages, two daughters with congenital ureteroceles and one healthy boy. This mode of inheritance is most consistent with an autosomal recessive pattern. Autosomal recessive diseases are associated with consanguineous marriage, due to the method of inheritance requiring two homozygous affected alleles. This further supports the genetic basis of familial ureterocele in terms of ureteral development. There is a special interest in ureteroceles which ‘run’ in families which has prompted many studies. One such study published in The Turkish Journal of Pediatrics concluded that the link between the inheritance and ureteroceles was autosomal dominant as opposed to recessive.4 This gives us a clue that there may be multiple types of inheritance pattern for this condition, which warrants further studies and analysis of genetics.
We have presented a rare case of familial ureterocele. The diagnosis was made during the morphology scan, however, the diagnosis could have been made earlier if she was seen at the feto -maternal center earlier based on her family history. Close collaboration between the attending obstetrician, feto-maternal specialist, pediatrician, radiologist and pediatric surgeon resulted in satisfactory outcome. In future pregnancies the patient may benefit from Prenatal Genetic Diagnosis (PGD), as it may possible to identify the affected gene by studying genetic work up of affected siblings and their parents.
None.
Author declares that there is no conflict of interest.

©2017 Al-Abdulmalek1, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.