eISSN: 2471-0016


The granular cell tumors are uncommon, mostly benign neoplasm of neural differentiation that can occur at any site of body. The diagnosis of the GCTs requires histopathological examination of the excised lesion. We present a histopathology case report of a GCT tumor in 26 year old female. Morphology of the tumor on Hematoxylin and Eosin (H&E) stained section, result of PAS stain, immunohistochemistry findings and differential diagnosis are discussed. Final report should include a comment on status of surgical margins because assessment of the surgical margins is important for GCTs as complete surgical excision is curative for almost all cases of benign GCTs.
Keywords: granular cell tumor, hematoxylin and eosin, smooth muscle actin
GCT, granular cell tumors; H&E, hematoxylin and eosin; NSE, neuron-specific enolase; SMA, smooth muscle actin
The granular cell tumors (GCTs) are rare benign soft tissue neoplasm of nerve sheath origin.1 They can occur at any site of the body. The GCT incidence is slightly higher in female. The GCTs usually occur in adults, uncommon in children, but very rarely they can occur as congenital disease. The most common site is the tongue, followed by other head & neck sites, anterior and posterior chest walls, upper limb, breast, GIT and lower limb. The granularity of the tumor cells is due to accumulation of secondary lysosomes in the cytoplasm.2,3 This finding is non-specific and occurs in many non-neural neoplasms and non-neoplastic conditions. Knowledge and understanding of full histopathological features and immunohistochemistry (IHC) findings are needed for accurate diagnosis of GCTs. This case report describes histopathological features with IHC finding of GCT that occurred in the subcutaneous tissue of elbow of a 26 years old female.
An excision biopsy specimen from a mass at elbow of 26 years old female patient was received for histopathological examination. The clinical impression was of ‘benign soft tissue tumor’. The specimen was received in 10% formalin in one container. On gross examination, it was a 1.5 x 1 x 0.5 cm well-circumscribed, grey-tan mass, without skin component. The cut surface was solid homogenous and no necrotic or hemorrhagic areas were found on it. The microscopic examination revealed a circumscribed encapsulated lesion composed of round to polygonal to spindle shaped cells with eosinophilic granular cytoplasm and centrally placed small nuclei (Figure 1 & Figure 2). Cells were arranged in intersecting bundles and mixed with fibrous connective tissue (Figure 3). The Intralesional peripheral nerve bundles surrounded by the lesional cells were seen (Figure 4). No significant mitoses or cells with cross striation, significant inflammatory infiltrate or necrosis were seen. IHC showed positive results for S100 (Figure 5) and neuron-specific Enolase (NSE) (Figure 6). Smooth muscle actin (SMA) (Figure 7) and Myogenin were negative. CEA was focally positive. Periodic acid-schiff (PAS) stain showed PAS positive intracytoplasmic granules (Figure 8). The lesion was completely excised with <1mm safety margin. Focal entrapment of the adjacent fatty tissue was observed. Based on the above mentioned findings, diagnosis of granular cell tumor (GCT) was made.
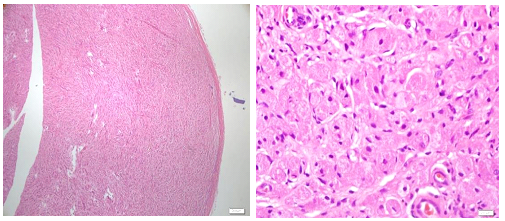
Granular cell tumor (GCT) is a rare tumor (Figure 1) and rarely diagnosed prior to histopathological examination of (Figure 2) the biopsy or excised specimen. The GCTs are usually poorly circumscribed and non-encapsulated. However, circumscribed encapsulated GCT can occur, especially in the skin and subcutaneous tissue. Reported cases of encapsulated GCTs are also present in the medical literature. The morphology of GCTs on H&E is easy to identify and it should be supported by PAS stain and IHC. PAS positive cytoplasmic granularity is a characteristic feature of the GCTs. GCTs are positive for S100, NSE, NK1-C3, vimentin, CD57 and CD68.1,4-7 The GCTs are non immunoreactive for epithelial, muscle, endothelial and glial cell markers. CEA positivity in some GCTs is a false positive result most likely due to non-specific cross reacting antigen in GCTs.
The histopathological differential diagnosis of GCTs includes atypical or malignant GCTs, rhabdomyoma, granular cell leiomyoma, hybernoma, xanthoma and reactive changes associated with trauma. Malignant GCTs are very rare, comprising <1% of total GCTs. The histologic criteria to differentiate the benign GCTs from their malignant counterpart include: presence of necrosis, spindling of the cells, vesicular nuclei with prominent nucleoli, nuclear pleomorphism, high N/C ratio and increased mitoses (>2/10 high power field).4,8,9 GCTs with three or more of these criteria are classified as malignant and as atypical if they have two of these features. The presented case showed (focal) spindling of the cells but without any other criteria of malignancy. We preferred to call it as benign GCT. The patient has recurrence free follow up for last four and half years. Absence of cross striations, presence of cytoplasmic PAS positive granules and S100 positivity differentiate GCTs from rhabdomyoma. Negative SMA and positive S100 rule out granular cell leiomyoma. PAS positive granules, S100 positivity and NSE positivity help to distinguish it from xanthoma. Absence of inflammatory infiltrate and IHC finding distinguish reactive lesion with granular cells from GCTs. Recommended treatment for GCTs is surgical excision with free surgical margins.5,10,11 Recurrence rate is very low for benign GCTs.
We would like to thank all three histotechnologists, Ms. Amna Essa, Ms. Loluwa and Ms. Shirin Murad for their hard work, interest in the subject and efficient performance to produce excellent quality of histopathology slides. We would also like to acknowledge the Surgical Department of Al Qassimi Hospital for its continuous support and trust in our department.
Both the authors have declared no conflict of interest for this work.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.