eISSN: 2373-6372


Case Report Volume 10 Issue 2
Hospital Nossa Senhora das Graças, Brazil
Correspondence: Katia Cristina Kampa, University : Hospital Nossa Senhora das Graças Address B.P: Alcides Munhoz, St, 433, Curitiba, Paraná, Brazil , Tel +55-41-988814273
Received: June 06, 2018 | Published: March 11, 2019
Citation: Kampa KC, Guerra JAAA, Percicotte AP, et al. Hepatic splenosis: a report of a very rare case. Gastroenterol Hepatol Open Access. 2019;10(2):88–91. DOI: 10.15406/ghoa.2019.10.00361
Splenosis is a heterotopic autotransplantation of splenic tissue after abdominal trauma or surgical intervention. Hepatic splenosis is very rare and the diagnosis is challenging, being confused with other benign and malign nodular hepatic lesions. As it is usually asymptomatic, most diagnoses are incidental. Despite being a rare condition, splenosis should be considered in differential diagnosis with other nodular hepatic lesions and accurate diagnosis is important to avoid unnecessary invasive procedures. Here we describe a case of a patient that underwent splenectomy 20 years ago, due to abdominal trauma. The patient was asymptomatic, without alteration in physical exam. The hepatic nodule was found on routine examination. The initial suspicion was of hepatic adenoma and therefore the patient underwent hepatectomy, with good clinical evolution. The definitive diagnosis was obtained only with anatomopathological analysis, characterized by the presence of splenic tissue in the hepatic parenchyma.
Splenosis is a benign condition, usually occurring after splenectomy, with implants of splenic tissue in other organs. The etiological differentiation of the nodules with the use of radiological and laboratory tests is difficult, and often the diagnosis is confirmed only after surgical procedure with anatomopathological study. The correct diagnostic definition is necessary and important because the differential diagnoses include hepatocellular carcinoma and other neoplasms, especially in patients with liver cirrhosis. Surgical treatment should be performed only if the diagnosis has not been defined or if there is complication due to the presence of splenic tissue in the affected organ.
Keywords: Hepatic splenosis, ectopic splenic tissue
Splenosis, one type of manifestation of ectopic spleen tissue,1,2 is a heterotopic autotransplantation of splenic tissue after abdominal trauma or surgical intervention (Figures 1). Hepatic splenosis is very rare, usually asymptomatic and cannot be distinguished from hepatic malignancies because of lack of significant radiological features.2,3 Therefore, suspicion is an important step for diagnosis and invasive procedures are usually necessary to establish a definitive diagnosis.
An important differentiation is made with hepatic adenomas, which are generally benign and, if smaller than 5 cm and asymptomatic, do not require surgical treatment, but if they are larger, they should be resected, due to the risk of hemorrhage or malign transformation.4
This was the initial suspicion in the presented clinical case and, therefore, the patient underwent surgical resection. Splenosis is a benign entity, but with several differential diagnoses and need for clinical correlation and images for correct definition.4–8 In patients with cirrhosis the most important differential diagnosis is with hepatocellular carcinoma and invasive procedures may be necessary for the definition.4,9 In this article we describe a clinical case of hepatic splenosis, its differential diagnoses and review of imaging methods for diagnostic definition.
Male, 47 years old, with an incidental finding of hepatic lesion, during investigation of nephrolithiasis. Previous history of splenectomy after abdominal trauma due to automobile accident 20 years ago. Hypertensive in use Olmesartan, denied other pathologies and surgeries. On physical examination: good general condition, anicteric, painless abdomen, without palpable masses. Laboratory tests: Hb 14g/dL (13,5 - 17,5), Hct 44,4% (39 - 55), Platelets 268,000/mm3 (150.000 - 400.000), creatine 0,9mg/dL (1,5), INR 0,8, CEA 1,33 ng/mL (<3,0), CA 19-9 20U/mL (<37), AFP 1,5ng/dl (<7,22 ), albumin 4,19g/dL (3,4 – 4,8), AST 20U/L (17 - 55), ALT 18U/L (21-71), GGT 54U/L (15/73), AP 48U/L (38 - 126), total bilirrubin 0,57mg/dL (0,2 – 1,3). MRI showed nodular hepatic lesion, 42x41x28mm, slight hyperintense in T2, with contrast enhancement and washout in late phase, in segment II, without dilatation of biliary tract (Figures 2). The initial diagnosis was hepatic adenoma. Proceeded with hepatic segmentectomy, with good evolution. The surgical specimen referred to pathological anatomy and revealed hepatic splenosis (Figures 1).
Ectopic spleen tissue takes two forms, it is either congenital and presents as accessory spleens or an acquired condition, called splenosis.1 Acessory spleen is a congenital condition caused by embryologic failure of the fusion of the splenic primordium characterized by a dense, syncytial-like, mesenchymal thickening of the dorsal mesogastrium during fetal development.4 They are found in 10-40% of patients at autopsy, rarely exceed 1,5cm in diameter, usually solitary, rarely exceed 6 in number, most commonly located on the left side of the dorsal mesogastrium in the region of the splenopancreatic or gastrosplenic ligaments.6,10
Splenosis, one type of manifestation of ectopic spleen tissue,2 is a heterotopic autotransplantation of splenic tissue (Figure 1), generally after abdominal trauma or surgical intervention,6 and in this reported case the patient was also submitted to splenectomy after abdominal trauma. The first case of splenosis was reported in the English literature in 1939 by Buchbinder and Lipkoff.11 In 2014, Naoya Sato et al.4 described the first case of hepatic splenosis without previous abdominal trauma or surgery.4
Although splenosis is believed to occur in up to 67% of cases with splenic trauma, the true incidence cannot be estimated as it is usually an incidental finding during surgical exploration or autopsy.4,6,11 They have no characteristic shape, have no hilus and do not form a normal capsule.6,10 Patients are usually asymptomatic, what could lead to an underdiagnosed condition.1 On the other hand, hepatic splenosis is rare and around 30 cases of this condition are reported in the medical literature.4,12
In splenosis occur implantation of splenic fragments onto exposed vascularized peritoneal and intrathoracic surfaces, following splenic injury or elective splenectomy.7 The heterotopic implants of splenic tissue might help restore splenic function after splenectomy. They are prone to the same pathologic conditions affecting the spleen.13 The mechanism of splenic autotransplantation and regeneration is not well understood.4,14 There have been proposed theories suggesting mechanical trauma and splenic rupture releasing splenic pulp into the surrounding tissues as possible major processes.14,15 Kwok et al.16 hypothesized that 2 events can promote the development of hepatic splenosis: the migration of erythrocytic progenitor cells through the portal vein following traumatic splenic rupture and the erythropoiesis induction by local hypoxia of the liver.12,16
Splenosis can occur with either single or multiple nodules, upward to 400 in some cases, and found throughout the peritoneal cavity, most often in the mesentery and omentum,4,6 and will receive its blood by parasitizing the surrounding tissue.7 Extraperitoneal locations that can also be involved are the retroperitoneal, thoracic, subcutaneous, and intrahepatic regions.4
Chen X et al.2 in 2015 reviewed all 34 cases reported in literature and described that approximately 80% (27/34) of patients diagnosed with hepatic splenosis had a history of splenectomy. The mean time interval between splenectomy and hepatic splenosis detection was 25 (1.5–47) years. The median size of reported hepatic splenosis is 30 mm in diameter. Previous reports also state that in more than half of the reported cases, hepatic splenosis was associated with chronic hepatitis C or B infection.4
Hepatic splenosis rarely has clinical significance4 and is usually asymptomatic, but complications have been reported, such as mass effect, acute abdominal pain due to obstruction caused by the lesion, bowel obstruction and invasion of the bowel wall, causing hemorrhage.6,10,15,17 The differential diagnosis is essential, as it will completely change the approach, treatment and evolution. However, it is challenging and difficult and should encompass hepatic adenoma, haemangioma, focal nodular hyperplasia, lymphoma and hepatocellular carcinoma.7,10 Particularly in patients with liver cirrhosis, with aberrant α-fetoprotein values and a background of hepatitis virus infection, it is more difficult to make a correct differential diagnosis of hepatic splenosis from hepatocellular carcinoma.10 In Ultrasound, Computed Tomography and Magnetic Ressonance, splenosis has the same appearance as the normal spleen.11
Intrahepatic splenosis shows increased enhancement on CT or MR images during the arterial phase. Performing gadoxetic acid–enhanced hepatocyte-phase MR imaging does not help because intrahepatic splenosis is hypointense during the hepatospecific phase. The MR technique involving administration of small iron oxide particles (SPIO-Endorem), which is taken up by liver and spleen reticuloendothelial cells, has proven to be effective in differentiating intra-hepatic splenosis from other lesions.14,15,18 With SPIO (superparamagnetic iron oxide) intrahepatic splenic nodes remain hyperintense.19 Noncontrast CT reveals a well circumscribed iso- or hypodense mass in the liver, while noncontrast MRI demonstrates mild-to-moderate hyperintensity on T2-weighted image and hypointensity on the T1-weighted image. A dynamic study on CT and MRI shows a slight to intense enhancement, which may be homogeneous or heterogeneous during the arterial phase but enhancement is diversely during the portal venous and equilibrium phases in different cases. Compared with the surrounding hepatic parenchyma, the lesion could reveal hypodensity and hypointensity, or hyperdensity in the arterial phase. Or it can demonstrate diminished enhancement, slight enhancement, or increased enhancement during the following phases (Figure 2 & 3).19,20
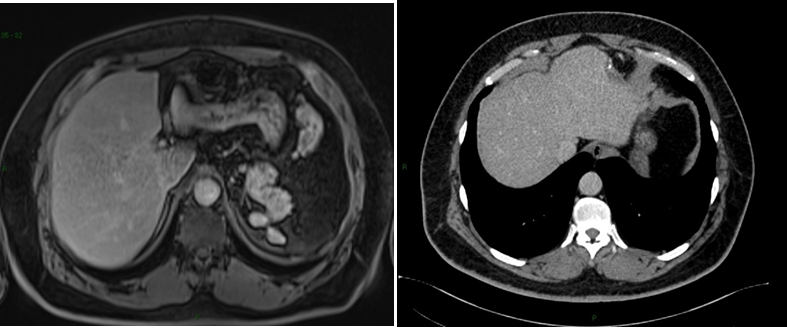
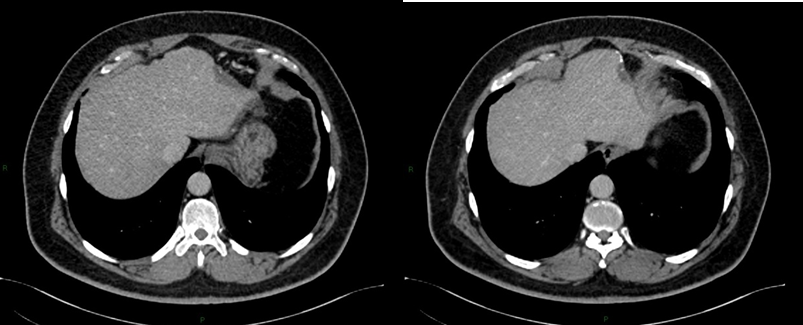
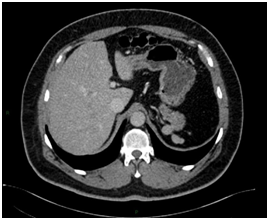
Figure 2 Magnetic Resonance Imaging (MRI). T2-weighted (A and B) and T1-post-contrast (C, D and E) images, in axial (A, C, D and E) and coronal (B) planes, that demonstrate subcapsular nodule in liver segment II, with intermediate sign in T2, enhancement in the post-contrast arterial phase (C) and washout with capsular enhancement in the venous phase (D). Signs of splenectomy and small implants of splenic tissue in the left subphrenic region (E) are also noted.
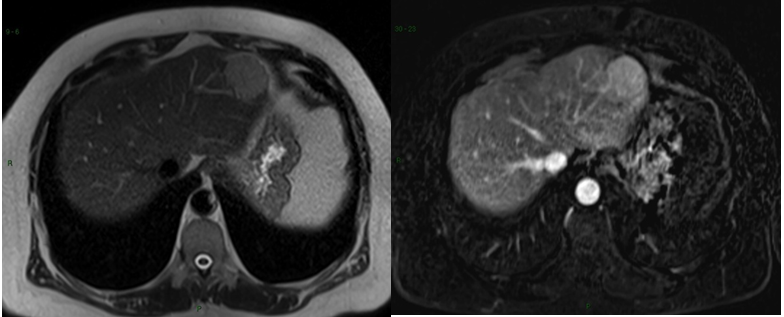
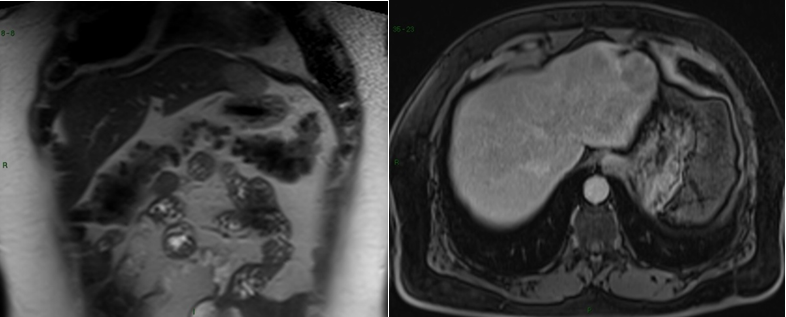

Figure 3Postoperative figures A, B, C, D and E. Computed Tomography (CT). Postoperative CT in the axial plane in the post-contrast venous phase show signs of partial resection of the liver segment II (A,B, C and D), as well as splenectomy with small implants of splenic tissue in the left subphrenic region (E).
In standard imaging techniques, such as US, CT-scan, or MRI, the hepatic splenosis may mimic adenoma, hepatocellular carcinoma, or metastatic liver neoplasms.8,21 In the imaging studies, the diagnosis was not definitive and hence the need for an invasive procedure.
The keys to diagnose intrahepatic splenosis are knowledge of splenic injury, the subcapsular location of the lesion (mostly in the left liver lobe), and the association with other hypervascular intraperitoneal lesions.22 If intrahepatic splenosis is suspected, technetium-99m–labeled red blood cell scintigraphy should be performed and represents the most specific imaging technique.8,22,23 Histology represents the gold standard for the diagnosis.8,24 Sometimes, laparoscopy is necessary for biopsy. Histologically, liver splenosis presents as nodular lesions rich in lymphoid tissue and hematopoietic cells, no hilus and its blood supply is derived from surrounding tissues and vessels (Figure 3).5,12 Due to the lack of adequate reported cases, there's no consensus on a gold standard diagnostic approach to hepatic splenosis.14
One very important differential diagnosis is with hepatocellular carcinoma in the setting of cirrhosis, since these patients could undergo unnecessary liver transplantation.8 In cirrhotic patients, hepatic splenosis should be considered in the differential diagnosis of hepatocellular carcinoma in patients with a history of splenectomy, especially if the lesion is located near the liver capsule.8 This will help to properly select patients who are candidates for liver transplantation, avoiding misdiagnosis.
Splenosis per se does not require particular follow up with diagnostic imaging or other investigations.15 Hepatic splenosis in absence of any symptoms do not require clinical treatment.12,19 The current opinion is that when splenosis is diagnosed, surgical removal is recommended only in the case of symptomatic complicated splenosis and in patients with hematological disease for whom splenectomy is beneficial.12
Although intrahepatic splenosis represents an extremely rare condition, this diagnosis should be kept in mind, especially in patients with history of abdominal trauma with splenic involvement presenting with an isolated liver lesion. Moreover, the adequate diagnostic of hepatic splenosis, a benign condition which in most cases do not require treatment, can avoid unnecessary interventions such as biopsy, angiography, operation and liver transplantation.
None.
Authors declare no conflicts of interest.

©2019 Kampa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 IBS awareness month is April, which is very common syndrome globally, so to develop awareness about the irritable bowel syndrome (IBS), we are eager to publish articles to spread acquaintance to all our readers. So, take the opportunity in sending your valuable articles to raise alertness to the global people and also get the best discount of 30% for your submissions to our Gastroenterology & Hepatology: Open access (GHOA).
IBS awareness month is April, which is very common syndrome globally, so to develop awareness about the irritable bowel syndrome (IBS), we are eager to publish articles to spread acquaintance to all our readers. So, take the opportunity in sending your valuable articles to raise alertness to the global people and also get the best discount of 30% for your submissions to our Gastroenterology & Hepatology: Open access (GHOA).