eISSN: 2373-6372


Tuberculosis is endemic in Tunisia. One-third of the world’s population is infected with tuberculosis (TB), with intestinal TB representing the sixth most common presentation of extra-pulmonary TB [1]. The diagnosis of intestinal TB is a challenge for physicians due to its diverse clinical manifestations that mimic other infectious, autoimmune, and tumor disorders, and is thus rarely considered as the causative agent of disease. Therefore, a high index of suspicion is essential to reach the correct diagnosis.
We report 3 cases of colonic tuberculosis which illustrate the variety of background circumstances and clinical manifestations that it may comprise.
Case n°1
We present a 45-year-old male with medical history of pleural tuberculosis for which he was treated with rifampicin, isoniazid, ethambutol and pyrazinamide since 3 weeks. He was admitted to the general surgery department for a small bowel obstruction with abdominal pain, vomiting and abdominal distension.
Abdominal examination revealed a diffuse distension with loud borborygmi and a tender left flank. The rectum was empty. Abdominal x-ray in up-right position showed fluid levels in the bowel. Biological investigations revealed a white cell count of 12700/mm3.
CT scan with contrast revealed a segmental thickening of the last ileal loops, distended small bowel loops without a detectable transition point, a 2 cm mesenteric mass associated with many mesenteric lymph nodes and magma of ileal loops some of which were contiguous to the sigmoid colon in the pelvis (Figure 1).
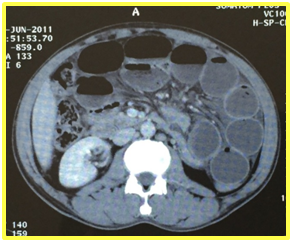
Figure1: A CT scan with contrast revealed a segmental thickening of the last ileal loops and distended small bowel loops without a detectable transition point.
A naso-gastric tube was placed on suction. There was no clinical improvement and surgical intervention was immediately prepared: the bowel obstruction was related to a mesenteric mass at which the small bowel and sigmoid colon were clustered and contiguous with dilation of the small bowel upstream. We performed a resection of the small bowel and sigmoid colon with the mesenteric mass. Pathological examination of the surgical specimen found a colonic tuberculosis fistulized in the mesentery (Figure 2).
He had an uneventful postoperative recovery and was discharged home with anti-TB medications. He remains asymptomatic 6 months following treatment with resolution of his symptoms.
Case n°2
A 21-year-old female was operated for an acute bowel obstruction related to a stenosis of the last ileal loop for which she had an ileo-cecal resection. Histological examination confirmed the diagnosis of ileo-cecal tuberculosis. She had a satisfactory evolution and was discharged. At 1 year follow-up she is doing well and has finished his course of anti-TB treatment.
Case n°3
An 18-year-old female presented with an intermittent diarrhea associated with peripheral and profound polyadenopathy. She had a colonoscopy with colonic and ileal biopsies. The mucosa of the left colon showed a pseudo-nodular appearance and was widely ulcerated in places. Anatomopathological examination found colonic tuberculosis. A treatment with anti-TB drugs was initiated and the outcome was uneventful [1].
Gastrointestinal tuberculosis is a quite common disease in our country, despite its prevention. Clinicians need to have gastrointestinal tuberculosis in their top diagnosis when dealing with patients with chronic gastrointestinal symptoms who are HIV-positive or coming from countries of high prevalence of TB. The signs and symptoms of intestinal TB are usually non-specific and diagnostic tests are sometime non-sensitive. A high level of evidence is required for an adequate diagnosis. Conservative management is successful in the majority of cases.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 IBS awareness month is April, which is very common syndrome globally, so to develop awareness about the irritable bowel syndrome (IBS), we are eager to publish articles to spread acquaintance to all our readers. So, take the opportunity in sending your valuable articles to raise alertness to the global people and also get the best discount of 30% for your submissions to our Gastroenterology & Hepatology: Open access (GHOA).
IBS awareness month is April, which is very common syndrome globally, so to develop awareness about the irritable bowel syndrome (IBS), we are eager to publish articles to spread acquaintance to all our readers. So, take the opportunity in sending your valuable articles to raise alertness to the global people and also get the best discount of 30% for your submissions to our Gastroenterology & Hepatology: Open access (GHOA).