eISSN: 2373-6372


Background and Aims: The prevalence of inflammatory bowel disease (IBD) is increasing rapidly in China. We aimed to explore the trends in epidemiological and clinical characteristics of IBD in Eastern China over the 15-year period.
Methods: This is a multi-center retrospective study. Newly diagnosed IBD cases from January 1995 to December 2009 (n=427) in Eastern China were included. Study protocol was approved by Institutional Review Board. Disease severity was assessed by Montreal classification. It was divided into two periods: 1995-2004 and 2005-2009. The epidemiological and clinical characteristics of ulcerative colitis (UC) and Crohn’s disease (CD) were compared in these two periods, respectively.
Results: The mean inpatient CD incidence had 2.5 fold increment with p<0.05 while incidence of UC did not change significantly over the two periods (p>0.05). The incidence growth of CD is significantly associated with the growth of gross domestic product (GDP) in China (P<0.001). There were no statistically significant difference regarding the mean age at diagnosis, gender ratio and mortality rate (P>0.05) between the two periods among both UC and CD. Meanwhile, the rate of applications of immunomodulators and biologics was higher in 2005-2009 than those in 1995–2004 (P<0.05).
Conclusions: During 1995 - 2009, age at diagnosis, gender and the familial occurrence of IBD did not change significantly in Eastern China. The incidence in inpatient CD has increased 2.5 fold and significantly associated with the GDP growth. This study provides insight into the possible local epidemiological and clinical patterns of IBD.
Keywords: change, epidemiology, clinical characteristics, inflammatory bowel disease
UC, ulcerative colitis; CD, crohn’s disease; IBD, inflammatory bowel disease; 5-ASA, 5-aminosalicylic acid; SASP, salazosulfapyridine; GDP, gross domestic product; SPSS, statistical product and service solutions
Ulcerative colitis (UC) and Crohn’s disease (CD) are two diseases under the umbrella of Inflammatory Bowel Disease (IBD). IBD has been traditionally considered a “western” disease. The highest annual incidence of UC reached 24.3 per 100,000 person-years in Europe, 19.2 per 100,000 person-years in North America, and 6.3 per 100,000 person-years in Asia and the Middle East, while that of CD was 12.7 per 100,000 person-years in Europe, 20.2 per 100,000 person-years in North America, and 5.0 person years in Asia and the Middle East.1 The incidence of IBD in Asia seems to be in a relatively low level, but it has progressively increased. A population-based study in Korea has indicated the mean annual incidence rates of CD and UC in 2001-2005 were increased by 25 and 8-fold, respectively, compared with those in 1986-1990.2 China has also experienced a steadily incidence growth with an 8.5-fold increase in 2002-2007 compared with 1989-1994, and there is a predominant annual increase in IBD since 2004.3 The increasing incidence of IBD is posing an emerging health issue in China, which has attracted much attention from gastroenterologists all over the country.4,5 However, long-term studies about the chronological changes in epidemiology and clinical nature of IBD currently are rare in China. In this study, we aimed to explore the trends in epidemiological and clinical characteristics of IBD in Eastern China. We analyzed 427 hospitalized patients diagnosed with IBD in 3 hospitals in Zhejiang province located in Eastern China from 1995 to 2009. Our study may provide an insight into the changing epidemiological and clinical patterns of IBD and offer potential opportunities to identify the etiological factors in Eastern China.
Patients
This study included all hospitalized newly diagnosed IBD cases in three hospitals in Zhejiang province located in Eastern China from 1 January 1995 to 31 December 2009. The three hospitals are geographically distributed in the west, north and east of Zhejiang province. 427 patients were enrolled. They all meet the Lennard-Jones criteria for diagnosis.6 Patients with a non-IBD diagnosis such as infectious colitis, bacillary dysentery, amebiasis, chronic schistosomiasis, intestinal tuberculosis, ischemic colitis and radiation colitis were excluded. The admission time of all patients were divided into two periods, 1995-2004 (A) and 2005-2009 (B). The patients were further categorized into two sub-groups within each period based on UC and CD forms (Group A1: UC, 1995-2004, n=116; Group B1: UC, 2005-2009, n=135; GroupA2: CD, 1995-2004, n=62; Group B2: CD, 2005-2009, n=114).
Assessment of diseases
Montreal classification7 was applied for both UC and CD. The extent of ulcerative colitis (UC) was classified as Ulcerative proctitis (E1), Left sided UC (E2), and Extensive UC (E3), while the severity of UC was divided into mild UC (S1), moderate UC (S2) and severe UC (S3). Patients with CD were classified by age of diagnosis (A1: ≤16 years; A2: 17-40years; A3:>40 years), location of disease (L1: ileal; L2: colonic; L3: ileocolonic; L4: isolated upper disease), and disease behavior (B1: non-stricturing, nonpenetrating; B2: stricturing; B3: penetrating; p: perianal disease modifier).
Data collection
In January 2000, we established an electronic database for all hospitalized patients in the three hospitals. It contained medical records from all of patients hospitalized thereafter. Additionally, paper medical records for all hospitalized patients between January 1995 and December 1999 from the medical record department were added to this database. Newly diagnosed IBD cases between 1 January 1995 to 31 December 2009 had been identified and their demographic, clinical profiles and treatment patterns had been collected retrospectively, including: gender, family history, age of diagnosis, severity, location, activity of disease, the laboratory examinations, the endoscopy, radiological, surgical and pathological records, the extra-intestinal manifestations and complications; the medication information of Salazosulfapyridine (SASP)/5-aminosalicylic acid (5-ASA), corticosteroids, immunomodulators and biological agents. Each patient has an individual medical records code, and for who had been hospitalized more than 2 times, only the first was taken into account.
The study design
This is a multi-center, retrospective and observational study. Data were extracted from the electronic database. Study protocol was approved by local Institutional Review Board. Clinical characteristics of the four groups mentioned above were compared. We compared epidemiological and clinical characteristics among the cases of each IBD type between two periods to seek potential shifts in epidemiological and clinical patterns.
Statistical analysis
The incidence in inpatients of IBD from 1995 to 2009 were calculated using the total number of new inpatients in the hospitals in one year as the denominator and the number of new cases of IBD inpatients of the same year as the numerator. The date when IBD was diagnosed rather than the date of symptom onset was used to determine incidence in inpatients in order to avoid recall bias. Incidence in inpatients was expressed as the number of patients per 1,000,000. Statistical analyses were performed by SPSS V 16.0 (Statistical Product and Service Solutions). The continuous data were expressed as mean values and standard deviation. The categorical data were expressed by percentages. One-way ANOVA test was performed to analyze the continuous data and the chi-square test or the Fisher's exact test was used to analyze the categorical data. Spearman rank correlation was used to identify the correlations between gross domestic product (GDP) and incidence in inpatients. P ≤ 0.05 was considered statistically significant.
Overall characteristics of IBD patients
251 (58.8%) UC and 176 (41.2%) CD patients were diagnosed during 1995-2009 in the three hospitals in Eastern China. All of them were ethnically Chinese. Their characteristics were summarized in Table 1 and Table 2.
UC (n = 251) Characteristics |
A1(n=116) |
B1(n=135) |
|
Male/female |
128/123 |
||
Median diagnosis age, years (range) |
48 (15-80) |
||
Extent n (%) |
|||
E1(Ulcerative proctitis ) |
27 (10.8) |
11(9.5) |
16(11.8) |
E2( Left sided UC ) |
105 (41.8) |
46(39.6) |
59(43.8) |
E3( Extensive UC ) |
119 (47.4) |
59(50.9) |
60(44.4) |
Severity n (%) |
|||
S1( Mild UC ) |
99 (39.5) |
46(39.7) |
53(39.3) |
S2( Moderate UC ) |
106 (42.2) |
50(43.1) |
56(41.5) |
S3( Severe UC ) |
46 (18.3) |
20(17.2) |
26(19.2) |
Clinical type n (%) |
|||
The initial |
76 (30.3) |
49(42.2) |
27(20.0) |
chronic relapsed |
153 (61.0) |
55(47.4) |
98(72.6) |
chronic persistent |
21 (8.3) |
12(10.4) |
9(6.7) |
The fulminant |
1 (0.4) |
0(0.0) |
1(0.7) |
Colectomy n (%) |
19 (7.6) |
11(9.5) |
8(5.9) |
Mortality n (%) |
1 (0.4) |
0(0) |
1(0.7) |
Family history n (%) |
1 (0.4) |
1(0.9) |
0(0) |
Drug therapy n (%) |
|||
SASP/5ASA |
226 (90.0) |
98(84.5) |
128(94.8) |
Corticosteroids |
103 (41.0) |
41(35.3) |
62(45.9) |
Immunosuppressive agents |
12 (4.8) |
1(0.9) |
11(8.1) |
Biological agents |
3 (1.2) |
0(0) |
3(8.1) |
Table 1 Characteristics of UC patients
Note: The distribution of clinical characteristics, the rate of colectomy, mortality, familial aggregation and the drug therapeutic status of IBD were calculated according to the number of inpatients.
CD (n=176) Characteristics |
A2(n=62) |
B2(n=114) |
|
1995-2004 |
2005-2009 |
||
Male/female |
105/71 |
37/25 |
68/46 |
Mean diagnosis age, years (range) |
34 (9-71) |
34.81±14.3 |
34.23±12.9 |
Age at diagnosis |
|||
A1(below 16 y) |
16 (9.1) |
6(9.7) |
10(8.8) |
A2 (17y-40y) |
116 (65.9) |
39(62.9) |
77(67.5) |
A3(above 40y) |
44 (25.0) |
17(27.4) |
27(23.7) |
Location |
|||
L1(ileal) |
45 (25.6) |
20(32.3) |
25(21.9) |
L2(colonic) |
37 (21.0) |
13(21.0) |
24(21.2) |
L3(ileocolonic) |
83 (47.2) |
25(40.3) |
58(50.9) |
L4(isolated upper disease) |
11 (6.2) |
4(6.4) |
7(6.1) |
Behavior |
|||
B1 (non-structuring, non-penetrating) |
97 (55.1) |
23(37.1) |
74(64.9) |
B2 (structuring) |
60 (34.1) |
28(45.2) |
32(28.1) |
B3 (penetrating) |
19 (10.8) |
11(17.7) |
8(7.0) |
P (perianal disease modifier) |
61 (34.7) |
17(27.4) |
44(38.6) |
Colectomy n (%) |
41 (23.3) |
20(32.3) |
21(18.4) |
Mortality n (%) |
4 (2.3) |
3(4.8) |
1(0.9) |
Family history n (%) |
3 (1.7) |
0(0) |
3(2.6) |
Drug therapy n (%) |
|||
SASP/5ASA |
162 (92.0) |
56(90.3) |
106(93.0) |
Corticosteroids |
82 (46.6) |
25(40.3) |
57(50.0) |
Immunosuppressive agents |
43 (24.4) |
8(12.9) |
35(30.7) |
Biological agents |
12 (6.8) |
0(0) |
12(6.8) |
Table 2 Characteristics of CD patients
Note: The distribution of clinical characteristics, the rate of colectomy, mortality, familial aggregation and the drug therapeutic status of IBD were calculated according to the number of inpatients.
Incidence of IBD in inpatients population over time and correlation with GDP
The overall incidence in inpatients of CD increased with 2.5 fold while the mean incidence in inpatients of UC displayed no significant difference (P>0.05). Meanwhile, the GDP grew steadily (Figure 1). The annual IBD incidence in inpatients and Gross Domestic Product (GDP) of Zhejiang province during 1995-2009 were shown in Table 3. The UC/CD ratio was decreased (P<0.05) from 1.87 in 1995 –2004 (group A1/A2) to 1.18 in 2005-2009 (group B1/B2). The incidence in inpatients of CD has caught up with or even surpassed that of UC since 2007. For Group A1 (UC 1995-2004, n=116) and Group B1 (UC 2005-2009, n=135), the mean hospitalization rates were 833/106 and 956/106 respectively. There was no significant increase in the hospitalization rates during the study period for UC (P=0.537). By contrast, for Group A2 (CD 1995-2004, n=62) and Group B2 (CD 2005-2009, n=114), the hospitalization rates were 383/106 and 954/106 respectively with the increment of 2.5 time (P=0.002). However, only the incidence in inpatients of CD (Figure 2b), instead of UC Figure 2(A), displayed a significant positive association with GDP (r=0.844, P<0.001).
Calendar Year |
Total hospitalization* |
IBD, n (/106) |
UC, n(/106) |
CD, n(/106) |
GDP (hundred Million yuan) |
1995 |
4,845 |
5(1032) |
4(826) |
1(206) |
3557.55 |
1996 |
5,930 |
2(337) |
2(337) |
0(0) |
4188.53 |
1997 |
8,312 |
2(241) |
2(241) |
0(0) |
4686.11 |
1998 |
10,341 |
7(677) |
5(484) |
2(193) |
5052.62 |
1999 |
12,656 |
15(1185) |
12(948) |
3(237) |
5443.92 |
2000 |
15,006 |
29(1933) |
21(1399) |
8(533) |
6141.03 |
2001 |
16,654 |
31(1861) |
21(1261) |
10(600) |
6898.34 |
2002 |
21,563 |
29(1345) |
14(649) |
15(696) |
8003.67 |
2003 |
23,307 |
46(1974) |
29(1244) |
17(729) |
9705.02 |
2004 |
26,657 |
42(1576) |
25(938) |
17(638) |
11648.7 |
2005 |
27,718 |
47(1696) |
24(866) |
23(830) |
13417.68 |
2006 |
30,828 |
68(2206) |
40(1298) |
28(908) |
15718.47 |
2007 |
33,765 |
70(2073) |
34(1007) |
36(1066) |
18753.73 |
2008 |
38,309 |
58(1514) |
33(861) |
25(653) |
21462.69 |
2009 |
44,177 |
91(2060) |
33(747) |
58(1313) |
22990.35 |
Table 3 The distributions of incidence in inpatients with IBD patients and the Gross Domestic Product (GDP) of Zhejiang province from 1995 to 2009
* Total hospitalization indicates the number of all hospitalization patients in the studied hospitals.
Note: The hospitalization rates of IBD were calculated according to the number of cases for patient admission.
Comparison of clinical characteristics
Disease location and severity
Extensive colitis (E3) and Left sided colitis (E2) were common for UC while proctitis (E1) was less common site Figure 3(A). The mild (S1) and moderate colitis (S2) accounted for about eighty percent of the UC cases Figure 3(B). There were no significant differences in terms of patterns of location (p=0.57) and severity (p=0.93) between the two periods, 1995-2004 and 2005-2009 (Figure 3a & 3b). However, the proportion of patients with relapse increased from 47.4% in group A1 (UC 1995-2004) to 72.6% in group B1 (UC 2005-2009). Conversely, the proportion of the initial type (Based on specific Chinese classification as: initial, chronic relapsed, chronic persistent and fulminant) decreased from 42.2% to 20.0% (Figure 3c, P<0.001). The distribution of location of CD was 32.2% ileal (L1), 21.0% colonic (L2) and 40.3% (L3) in group A2 (CD 1995-2004) while it was 21.9% (L1), 21.2% (L2) and 50.9% (L3) in group B2 (CD 2004-2009) Figure 4(B). The distributions of both age at diagnosis (P=0.82) and location (P=0.43) of CD remained unchanged Figure 4(A & B). The proportions of patients with non-stricturing/ non-penetrating behavior increased significantly, from 37.1% in group A2 to 64.9% in group B2, while the proportions of the stricturing decreased from 45.2% in group A2 to 28.1% in group B2; penetrating types were decreased from 17.7% in group A2 to 7.0% in group B2 Figure 4 (C), P=0.001).
Gender
Among UC patients, 58 males and 58 females were diagnosed during 1995-2004 (group A1), while 70 males and 65 females were diagnosed during 2005-2009 (group B1). Group A1and B1 displayed no significant difference in gender ratio (M/F: 1 vs 1.08, P=0.77). There were 37 males and 25 females in 1995-2004 (group A2), as well as 68 males and 46 females in 2005-2009 (group B2), were diagnosed with CD. The gender ratio of CD patients did not change significantly (M/F: 1.48 vs 1.48, P=1.0).
Age at diagnosis
The overall mean age at diagnosis was 47.53±14.1 years for UC, and 34.53±13.4 years for CD. The distribution of age at diagnosis showed a main peak in the fifth decade for UC (Supplemental Figure 1(A), and a main peak in the third decade for CD (Supplemental Figure 1(B). There was no significant change of age at diagnosis for either UC or CD between these two periods. In 1994-2004, the mean age at diagnosis of UC was 47.01±14.8 years, while it was 47.97±13.6 years in 2005-2009 (P=0.59). Similarly, the mean age at diagnosis for CD was 34.81±14.3 years in 1994-2004 and 34.23±12.9 years in 2005-2009 (P=0.78). 62.9% of CD patients in group A2 (CD 1995-2004) and 67.5% in group B2 (CD 2005-2009) were diagnosed between 17 to 40 years old Figure 4(A).

Figure 1 The trends of incidence in inpatients of IBD and Gross domestic product (GDP) in Zhejiang province with calendar year from 1995 to 2009.
Colectomy
Colectomy was performed in 19 UC patients and 41 CD patients. There was no significant difference for the colectomy rates of UC patients in 1995-2004 (9.5%) and 2005-2009 (5.9%) with P=0.29. By contrast, a lower colectomy rate of CD patient in 2005-2009 compared with the colectomy rate in 1995-2004 (18.4 vs 32.3% P=0.04).
Mortality
Only one death occurred in UC patients which was from group B1 (UC 2005-2009) and died from hepatic failure (patient had primary sclerosing cholangitis-UC). There were four deaths in CD patients. Three of them occurred in group A2 (1995-2004) and one of them occurred in group B2 (2005-2009) (0.048 vs 0.0087, p<0.01). In detail, causes for death were intestinal perforation (1), intestinal hemorrhage and hemorrhagic shock (2) and toxic megacolon (1). Therefore the mortality from CD significantly decreased from 1995-2004 to 2005-2009.
Family history
Only one female UC patients (from A1 1995-2004) had a family history of father being diagnosed of UC. No family history was reported in group B1 (2005-2009). There was no significant difference in familial aggregation between the two groups (P=0.46). Meanwhile, three CD patients from group B2 (2005-2009) had a positive family history, and no CD patients from group A2 (1995-2004) had positive family history.
Medications
Among UC patients, the applications of the Salazosulfapyridine(SASP)/5ASA, Corticosteroids, immunosuppressive and biological agents in group B1 were higher compared with group A1 (Supplemental Figure 2A, P<0.05). A similar tendency was observed in CD patients. The proportion of the SASP/5ASA, Corticosteroids, immunosuppressive and biological agents were increasing from group A2 to B2 (Supplemental Figure 2B, P<0.05).
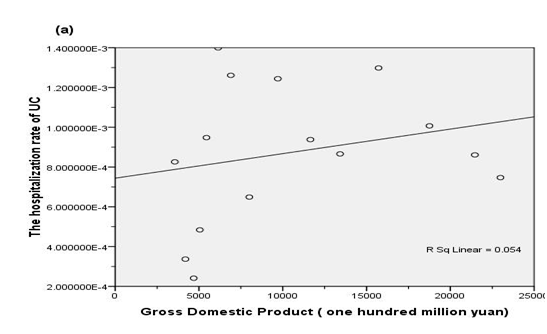
Figure 2 The association of gross domestic product (GDP) with incidence in inpatients of UC (a) and CD (b) patients
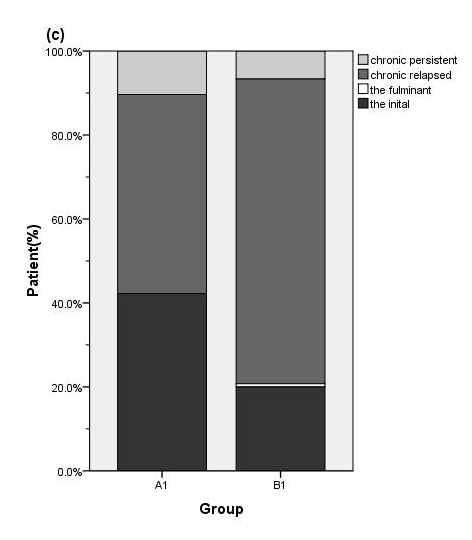
Figure 3 Distributions of the extent (a) severity (b) and clinical type (c) of UC according to the admission year (A1: 1995-2004; B1: 2005-2009). The proportion of chronic relapsed type increased while the initial type decreased during the study period. (P < 0.001)
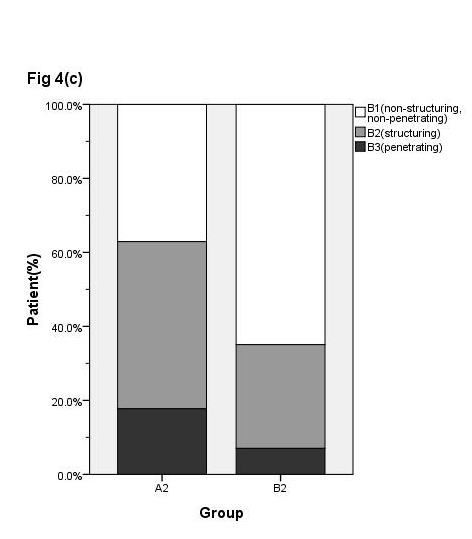
Figure 4 Distributions of the age (a) location (b) and behavior (c) of CD according to the admission year (A2: 1995-2004; B2:2005-2009). The proportion of B1 (non-structuring non-penetrating) increased while the B3 (penetrating) type decreased during the study period (P = 0.001)

Supplemental Figure 2 Drug therapeutic status of UC patients (a) and CD patients (b). The applications of SASP/5-ASA, corticosteroids, immunosuppressive agents and biological agents both increased in UC patients (P = 0.036 with Fisher's exact test) and CD patients (P = 0.018 with Fisher's exact test)
There are rapid increases of IBD cases in China during the last two decades. However, studies about chronological changes of IBD are scarce. In this study, we investigated the epidemiological and clinical characteristics trend in IBD patients based on our hospital registry database. The first large-scale multicenter study of hospitalized patients with IBD in China showed that the year-specific proportion of UC cases to all GI cases in 2001 was 2.11 times higher than in 1990.8 The year-specific ratio of CD to all hospitalized patients in 2003 was 2.78-fold higher than that in 1990.9 In our study, the highest annual incidence in inpatients of UC was 5.8 fold higher than the lowest. However, the mean rate of UC in 2005-2009 did not increase significantly than that in 1995-2004. By contrast, the growth of incidence in inpatients of CD was particularly remarkable. This shift tendency in UC/CD ratio was also seen in some Asian and Western countries. In Korea, the UC/CD ratio decreased from 6.8 in 1986-1990 to 2.3 in 2001-2005.2 In Olmsted, County, Minnesota, the prevalence of UC has decreased by 7% since 1991, while the prevalence of CD has increased by about 31%.10 In Hungary, a sharp increase in incidence of UC and CD were seen from 1977 to 2001 as the ratio of UC/CD incidence rates decreased from 4.05 to 2.35 during the observed periods.11 In northern France, the incidence of CD increased by 23% from 1988 to 1999, while that of UC decreased by 17% during the same period.12 All of the above suggested that the incidence of UC has reached a plateau phase while CD becomes more prevalent. With the increasing incidence of IBD in China, the gap of incidence rates between China and western countries is diminishing.
GDP is used to measure the economic conditions of one country. In our study, we found the incidence in inpatients of CD was consistent with the GDP growth, suggesting that the environmental factors may play a role in the pathogenesis of CD. With the social and economic development in Zhejiang province in the past two decades, the emerging western lifestyle such as diet habit, increasing industrialization and urbanization may provide valuable clues to the increment of IBD. In addition, the better diagnostic techniques, the improvement in livelihood and healthcare, and the increased physician awareness of this disease have promoted the detect capability of CD cases. This phenomenon was also seen in some other Asian countries. The incidence rate of IBD increased rapidly in Japan in the 1960s and 1970s,13 and in Korea the increase was seen in 1980s and 1990s.14 In American, the incidence and prevalence of CD has increased since the Second World War.15 It may test the hygiene hypothesis that there has been a fundamental change from a "dirty" lifestyle with high microbial exposure, to a "clean" lifestyle with low microbial exposure.16 The location of IBD in our study did not change obviously during the past 15 years, similar to our previously study in 2003.17 The pancolitis was the most common site of UC, while proctitis was less common. The most frequent locations of CD were the ileum and colon. These results are consistent with studies performed in Hong Kong, Japan and America.15,18,19 But in a Korean and some western population-based studies, the most frequent location of UC was proctitis.2,20 This discrepancy may be related to selection bias due to the fact that our study and some selected studies in Asia were hospital-based and may have not included all patients with mild UC. According to our data, the most commonly reported phenotype of CD was the behavior of penetrating type during 1995-2004, while during the 2005-2009, it was the behavior of non-penetrating and non-stricturing. This result is similar to an American study, in which the prevalence of the inflammatory phenotype was significantly greater than stricturing disease (65% versus 16%, OR 4.1, 95% CI: 2.5-7.0, P=0.001) or fistulizing disease (65% versus 19%, or 3.4, 95% CI: 2.1-5.5, P=0.001).21 This might be related to the development of economy and the level of medical care in the corresponding area. Patients may seek medical care earlier in the course of the disease before it gets complicated with penetrating or stricturing.
In our investigation, there was no significant change in the gender ratio and mean age at diagnosis during the past 15 years. The equal gender distribution for UC in our study was similar to the studies in Asia and western countries, whereas there appears to be male predominance for CD in China and in other Asian countries. This is in contrast to western studies that generally show an equal gender distribution or a moderate female predominance for CD. The reasons for gender differences between Asian and western are unclear but may be related to smoking or genetic factors. The mean age at diagnosis of UC and CD was 48 years and 34 years respectively in our data. While in Western studies, UC is diagnosed most frequently in patients in the 30-40 year-old age group, but CD tends to be diagnosed most frequently in the 20-30 year-old group.22 We found that the colectomy rate of UC was 7.6% without significant changes during the last 15 years. It is comparable to the long-term follow-up study of Hong Kong which showed the cumulative colectomy rates were 2.4 % and 7.6 % at 1 and 10 years of follow up.18 In a recent Korean study of UC cases diagnosed from 1989 to 2005 reported lower cumulative colectomy rates of 2.0% after 1 year, 2.8% after 3 years and 3.3% after 5-15 years.23 In South-Eastern Norway, the cumulative colectomy rate was 3.5%, 7.6%, and 9.8% after 1, 5 and 10 years.24 The rate of colectomy was significantly lower in China compared to some Western countries with colectomy rates of 3-10% after 1 year, 8 -20% after 5 years, and 24-34% after 10 years.20 The colectomy rate of CD in our investigation showed a significant decreasing tendency from 32.3% in the period of 1995-2004 to 18.4% in 2005-2009, which was lower than the studies in Japan and western countries. A recent Japanese study reported that the cumulative colectomy rate of CD was 37.6%, 60.4% and 74.2% at 5, 10 and 15 years after the onset of symptoms, respectively.25 In South-Eastern Norway, 28% of CD patients underwent intestinal resection during the 5 years follow up.26 In Olmstead County, Minnesota, 41% of CD patients underwent one or more surgical procedure during follow up.27 In western countries, the cumulative colectomy rate of CD was 40%, 60%, 70% and 90% at 5,15 ,20 and 30 years respectively.25,28 The lower colectomy may be due to many reasons including the milder disease, the short duration of follow up, a better response to medical therapy, the reluctance attitude toward the colectomy by both patients and surgeons. The UC-related mortality was 0.4% in our investigation without any changes during past 15 years. The mortality tendency of UC was similar to North American. In Olmsted County, Minnesota in 1940-2004, the cumulative survival of UC were 93%, 85%, 72% and 59% after 10, 20, 30 and 40 years. The cause specific mortality was not significantly increased in any subcategory. By contrast, a decreased mortality from cardiovascular disease was observed in UC.29 Our data showed the mortality of CD was 2.3%, and was decreasing from period of 1995-2004 to 2005-2009, which is similar to a tendency observed in Olmsted County, Minnesota during 1940-2004.15,29 Meanwhile, we have noticed the GDP was increasing and the drug therapeutic status was improving, suggesting the improvement of health service and treatment strategies might contribute to the reduction of the CD-related mortality. The familial aggregation rates for UC and CD in our study were 0.4% and 1.7% respectively, without any significant changes during the study period, which is much lower than the reported rates ranging from 8% to 14% in western countries.20 A Korean study showed that the frequency of familial history may rise with time, in parallel with the increase in prevalence of IBD within the country.2 However, we did not find this trend in China.
Our results showed the drug treatment strategies were improving as standard treatments were implemented with the improved physician awareness and as new drugs were developed with the advanced research on pathogenesis of IBD. Various therapy options have been available. The curative effects have shift from improving symptoms to mucosal healing. For example, the novel biological agent, infliximab has been regularly used in studied hospitals since 2009, with 15 patients prescribed infliximab just in 2009. However our hospital-based study has its limitations as it may have not included all patients with mild IBD and thus is less accurate than a population-based study. Though we have reported the medications, the prognosis of IBD needs further investigation.
In conclusion, during 1995-2009, the age, gender, location distribution and the familial occurrence of IBD did not change significantly in eastern China. The incidence in inpatients of CD has increased and significantly associated with the GDP growth. Whereas, the decreasing tendency of colectomy and mortality rates were similar to western countries, as standardized treatment of IBD are being implemented in China. This study provides insight into the possible local changing epidemiological and clinical patterns of IBD. But further population-based and long-term follow-up studies are still required in China to obtain nationwide epidemiological information.
None.
The author declares there is no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 IBS awareness month is April, which is very common syndrome globally, so to develop awareness about the irritable bowel syndrome (IBS), we are eager to publish articles to spread acquaintance to all our readers. So, take the opportunity in sending your valuable articles to raise alertness to the global people and also get the best discount of 30% for your submissions to our Gastroenterology & Hepatology: Open access (GHOA).
IBS awareness month is April, which is very common syndrome globally, so to develop awareness about the irritable bowel syndrome (IBS), we are eager to publish articles to spread acquaintance to all our readers. So, take the opportunity in sending your valuable articles to raise alertness to the global people and also get the best discount of 30% for your submissions to our Gastroenterology & Hepatology: Open access (GHOA).