Journal of
eISSN: 2373-6410


Mini Review Volume 6 Issue 5
1Department of Genetics, Faculty of Biology of Lomonosov Moscow State University, Russia
2University diagnostic laboratory, Russia
Correspondence: Eugene Klimov, Department of Genetics, Faculty of Biology of Lomonosov Moscow State University, 119234, Moscow, Lenin Hills, 1-12, Russia
Received: February 14, 2017 | Published: May 5, 2017
Citation: Klimov E (2017) Facioscapulohumeral Muscular Dystrophy: The Molecular Signaling Pathway. J Neurol Stroke 6(5): 00216. DOI: 10.15406/jnsk.2017.06.00216
Facioscapulohumeral muscular dystrophy (FSHD) is the third most common myopathy found in adults. It is a unique genetic disease because the activation of the normally inactive gene leads to the development of pathology. The molecular mechanisms and the signaling pathways remain poorly studied so far. Here the literature data is summarized and the molecular signaling pathway of FSHD is reconstructed.
Keywords: Facioscapulohumeral muscular dystrophy; FSHD; DUX4; Signaling pathways
FSHD: Facioscapulohumeral Muscular Dystrophy
Facioscapulohumeral muscular dystrophy (FSHD) is the third most common myopathy found in adults, with an overall incidence of more than 1:20000 (source: Orphanet). It is classified among progressive muscular dystrophies, characterized by muscular fiber necrosis and degeneration giving rise to progressive muscular weakness and atrophy. Weakness usually progresses very slowly, allowing FSHD patients to adapt and compensate muscular deficiencies, at least at the functional level [1].
This is the only case in which the activation of the normally inactive gene leads to the development of pathology [2,3]. But molecular mechanisms of this pathology are still unclear. Here I try to summarize the literature data and reconstruct the molecular signaling pathway of FSHD.
In most patients, FSHD is inherited as an autosomal dominant trait (FSHD1) and de novo cases are accounting for around 25% of patients. De novo cases are often in the mosaic form. Linkage studies on large families have mapped the disease locus to the subtelomeric region of chromosome 4, more specifically at 4q35-qter. This chromosomal region lacks classical genes but contains a macrosatellite repeat comprised of an array of repeated 3.3 kb units, named D4Z4 [4]. Analysis carried out in the past of a large population of healthy subjects and FSHD patients established that the number of D4Z4 repeated units on chromosome 4 varies in the general population between 11 and 110, whereas FSHD patients carry a contracted allele from 1 to 10 repeated units [5].
A small proportion of patients (around 5-10%) with features of FSHD do not harbor a contraction of the 4q35 D4Z4 array and they often have a complex pattern of inheritance - the second form of FSHD, termed FSHD2. FSHD2 patients were shown to harbor heterozygous mutations in SMCHD1 gene on chromosome 18p11.32. This gene is essential for the inactivation of the X chromosome (by interacting with DNA) and binds with cytosine-5-methyltransferase DNMT3B [6]. Mutations apparently cause a loss of function of the protein and the pathogenesis of the disease is likely due to SMCHD1 haploin sufficiency. Therefore FSHD2 is a digenic disorder, which requires both a loss-of-function mutation in one copy of SMCHD1 and a permissive 4qA allele. The lack of activity of SMCHD1 cannot effectively set the de novo methylation of the D4Z4 locus [7].
To reconstruct the signaling pathways I used Pathway Studio 9 ® software and abstract database ResNet12 ® by Elsevier. ResNet12 ® database contains information from literature sources freely available on the Internet, as of December, 2015. The signaling pathway of FSHD is presented on the figure. The data from experiments using biopsies, patients’ cell cultures model and mouse FSHD model was used (Figure 1).
The muscle fiber necrosis and degeneration occurs due to activation of transcription of DUX4 gene [8]. Genes FRG1 and FRG2 are adjacent to DUX4 [9,10]. FRG1 activation leads to increased activity of spliceosome. Also, with use of mouse model of FSHD, it was shown that FRG1 reduces the stability of mRNA of RBFOX1 [11], which plays an important role in alternative splicing - binds to exon-intron recognition motifs. Thus, the splicing process is activated, but the accuracy is reduced. This apparently leads to accumulation of abnormal splicing products, which adversely affects the cell cycle. Also FRG1 positively affect the passage of the cells in G1 phase in mouse model of FSHD [12]. The role of the gene product FRG2 is not clear yet.
The transcription factor SP1 is also a target of DUX4 [13]. Its activation is required for transcription initiation of CDKN1A, which, in turn, blocks the cell cycle at the G1 phase. Also DUX4 regulates the transcriptional activity of PITX1 gene [14]. Protein PITX1 itself is a transcription factor for TP53. The increase of the TP53 expression leads to blocking of muscle cell differentiation and apoptosis. Also TP53 binds the promoter of TP53I3 gene, regulating its expression. TP53I3 itself binds to the promoter of plasma glutathione peroxidase 3 (GPX3), adjusting its transcriptional activity. GPX3 reduces oxidative stress by the degradation of H2O2.
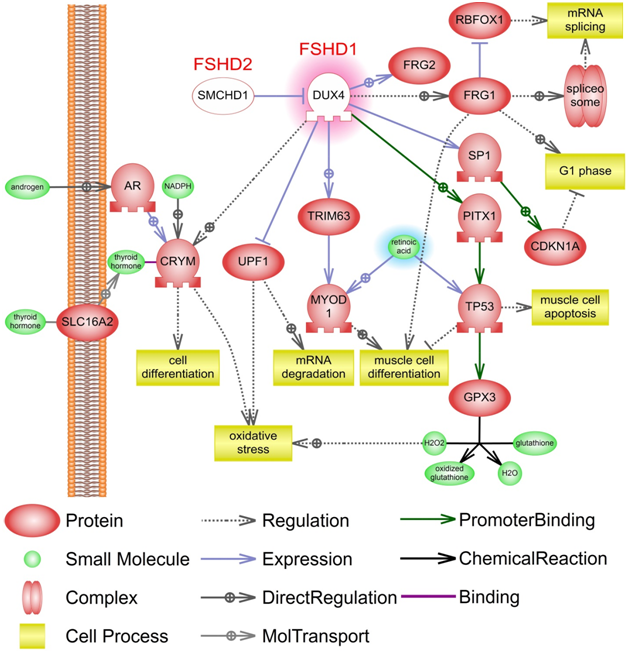
Figure 1: The molecular signaling pathway of facioscapulohumeral muscular dystrophy (FSHD). DUX4 with red highlights have increased expression. Mutated DUX4 and SMCHD1 are shown in white-out style. Retinoic acid with blue highlights has reduced concentration. A detailed description is provided in the text. Legend is on figure. Designed in the Pathway Studio 9 ® (Elsevier). This signaling pathway is built manually using published studies.
TRIM63 and FBXO32 are other expression targets of DUX4. TRIM63 protein is an E3 ubiquitin ligase that localizes in the Z-line and M-line lattices of myofibrils. This protein plays an important role in the atrophy of skeletal muscle and is required for the degradation of myosin heavy chain proteins, myosin light chain, myosin binding protein, and for muscle-type creatine kinase (CKM). FBXO32 contains an F-box domain and belongs to the Fbxs class, which plays role in phosphorylation-dependent ubiquitination. This protein is highly expressed during muscle atrophy. TRIM63 enhances specifically the proteolysis of myofibrillar protein and FBXO32 contributes to reduce muscle protein synthesis. TRIM63 and FBXO32 both negatively regulate the expression of MYOD1 protein, activate its ubiquitination and turnover. This leads to blockage of muscle cell differentiation[15,16].
Protein UPF1 subjected to proteolytic degradation with the participation of DUX4 [17]. UPF1 protein itself is involved in oxidative stress response; also, UPF1 is a trigger of mRNA degradation and participates in cell differentiation. The mu-crystallin protein (CRYM) is activated in the presence of DUX4 protein [14]. Mechanisms of CRYM activation are unknown. However, its direct regulators are androgen receptor (AR) and thyroid-hormone. CRYM protein influences on differentiation and oxidative stress responses. Also FSHD is characterized by a lack of retinoic acid [18], which regulates MYOD1 [19] and TP53 [20].
Facioscapulohumeral muscular dystrophy is the unique genetic disease. The molecular mechanisms and the signaling pathways remain poorly studied so far. With help of the mouse model of FSHD and cultured cells from patients we can better understand the molecular mechanisms of this disease, as well as the mechanisms of pathogenesis of other myodystrophies and the functioning of skeletal muscles. Meanwhile, it is now clear that the repression of DUX4 gene will block the negative signaling pathways. This repression can be carried out with the use of gene-silencing approach for example.

©2017 Klimov. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.