Advances in
eISSN: 2377-4290


Research Article Volume 4 Issue 3
Ivano-Frankivsk national medical university, Ukraine
Correspondence: Natalia Moyseenko, Ivano-Frankivsk national medical university, 118 Galitska 13, Ukraine, Tel +380677566341
Received: December 04, 2015 | Published: May 24, 2016
Citation: Moyseenko N. Optimization of neuroprotective therapy for compressive traumatic optic neuropathy. Adv Ophthalmol Vis Syst. 2016;4(3):75-77. DOI: 10.15406/aovs.2016.04.00109
As a rule, the posttraumatic optic nerve atrophy is evoked by its compressive damage. The purpose of the study is to increase the efficiency of treatment of optic neuropathy caused by traumatic orbital fracture compression using neuroprotective therapy. Six patients with optic nerve compression injuries were examined for clinical research. The neuroprotective support with corticosteroids had been used before and during surgical treatment as well as in the early postoperative period.
One of such example is a patient G with multiple fractures at the lower and outer walls of the orbital with displacement in the region of the orbit apex. His preoperative visual acuity decreased (to 0.04) in the damaged eye and (to 0.6) on the opposite side. Three months after injury vision acuity in both eyes was 1.0. Thus, the use of steroid as neuroprotective support for compressive traumatic optic neuropathy may help to protect the optic nerve from possible repeated injuries. Optimizing treatment regimen will increase the effectiveness of clinical outcome in general.
Keywords: traumatic impairment of the optic nerve, neuroprotective therapy, corticosteroid
TON: traumatic optic neuropathy’s; CT: scanned computer; MRI: magnetic resonance imaging
The posttraumatic optic nerve atrophy is often evoked by its compressive damage.1 Closed traumatic brain injury causes such complications in 43.1%.2 However, the most serious consequence for compression optic nerve damage is occurring in 2.5% of maxillofacial trauma.3 The traumatic optic neuropathy’s (TON) prognosis for functional recovery is doubtful if orbital fractures are present. The situation is better if fractures located in anterior part of the orbital cavity without dislocations. Nevertheless, multiple fractures in the posterior part close to the orbital apex are more dangerous.4 They may cause optic nerve compression in the canal, with the following damage in the blood vessels and secondary dystrophy of nerves fibers and surround tissues injury, which leads to atrophy of the optic nerve and incurable blindness.5
The most effective method of compressive TON treatment is decompression surgery.6 Nevertheless, surgical treatment for traumatic optic neuropathy sometimes can cause iatrogenic injury in the optic nerve. In particular, reducing of strangulation and displacement of zigomo-maxillary fissure may lengthen it to the optic nerve canal.7 Also during the reconstruction, surgical operations produce more movement, stretching, and torsion to the orbital bones that are additional injury factors to the optic nerve. That is why TON treatment by surgical method is not perfect.
It is generally accepted that the combination of conservative and surgical intervention is better. Decompression surgery should be used within 7 days after the trauma, but injection of methylprednisolone should be started as soon as possible. Also it is shown that the decompression endoscopic operations have positive effect if it is combined with methylprednisolone for 72 hours during the gradual reduction of corticosteroids.3 Therefore introducing neuroprotective therapy may reduce the risk of recurrent iatrogenic injury following the reconstruction operation to the traumatic eyes. The purpose was to maximize the neuroprotective therapy for compressive traumatic optic neuropathy.
Six clinical cases of our experience in treatment of optic nerve compression due to orbital fracture displacement were confirmed by spiral computer tomography and followed up in Ivano-Frankivsk regional hospital, Ukraine. In the first days eye examinations included determination of pupillary and eye movement reactions and ophthalmoscopy. After stabilization, mobility and response were evaluated. Three months after treatment, we examined visual acuity, visual fields and the limit of the electronic sensitivity (Phosphene). As methods for optical visualization on compressive nerve damage we used the spiral scanned computer (CT) and magnetic resonance imaging (MRI).
First patient A., female, had anisocoria with slow and weak direct light reaction on the affected side. The optic nerve injury was suspected. Her CT confirmed multiple orbital cavity dislocation fracture with optic nerve compression. Reconstructive osteoplastic surgery was made in three weeks after injury (because of her general bad condition) without steroid therapy before. Nerveless, secondary examination on the next day after surgery (one month after injury) showed absence of response that proved reducing of functional symptoms and indicated possibility of iatrogenic incurable damage to the optic nerve. After three months suspicions were confirmed in conscious patient based on visual acuity 0.0 (zero).
Second patient B., man, (Figure 1) was followed in unconscious condition in the hospital. The primary examinations detected ophthalmoplegia, paralytic strabismus, ptosis, violation of convergence. The superior orbital fissure damage and optic nerve compression were diagnosed. Plastic state was performed one month after the injury. He was observed by ophthalmologist one week after surgical treatment. His visual acuity on the affected side was 0.0 (zero), on opposite side was 0.8. Absence of perception light remained preserved, although little direct reaction of the pupil to light on the affected side was saved. IV infusion of Methylprednisolone at dose of 1000 mg/day was used for three days, followed by gradual reduction of the dose. Phosphine-stimulation was used after two weeks. After full course of treatment his visual acuity ipsilateral side has not changed, but on the contrary - increase to 1.0. His visual field expanded and electrical performance sensitivity of the optic nerve improved.
Figure 1 CT scan of right orbit of patient B.: the right orbit dislocation fracture of medial wall (1), right optic nerve compression (2) associated with upper fissure orbit damage (3). Examinations detected ophthalmoplegia, paralytic strabismus, ptosis, violation of convergence. The superior orbital fissure damage and optic nerve compression were diagnosed. Visual acuity on the right side was 0.0 (zero), on the left side was 0.8. The light perception is absence. Direct reaction of the pupil to light on the affected side saved.
Patients F and L (Figure 2) were in better general condition. The damage of the orbital bones in the apex with retrobulbar hematoma appeared in the early stages. They had blurring of vision and bilateral central scotomas. They received the same steroid neuroprotection as patient B. Their visual acuity became better (0.8 in affected side and 1.0 in opposite) in four months. The question of surgical treatment remains open under lesions in the top area of the orbit, a possible high risk of injury to the optic nerve. One more patient S started his treatment from Methylprednisolone in dose 1000 mg. He took Phosphine-stimulation after two weeks. His examination after the first four months showed that his visual acuity on the right (affected) eye increased from 0.4 to 0.8. On the left side (opposite), visual acuity has become better also, from 0.8 to 1.0. However, his eye movement is limited. He had double vision, corrected by prism lens. Therefore, given the high risk of re-injury of the optic nerve, the issue of plastic orbit remains currently open.
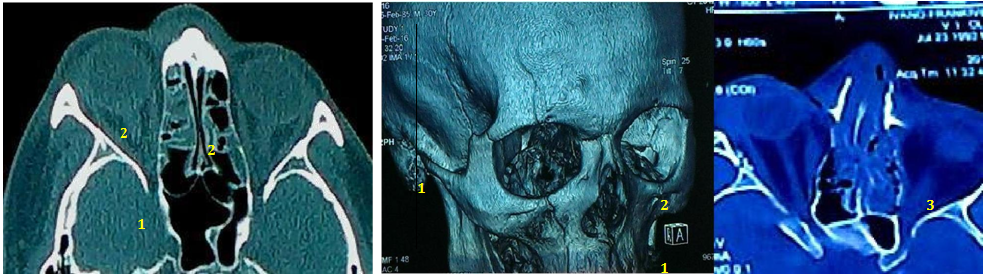
Figure 2 CT scan of patient F. and L. (the last): the right orbital multiple bones fractures with apex dislocation (1), bilateral optic nerve swelling (2) and left retro bulbar hematoma (3). The damage of the orbital bones in the apex with retrobulbar hematoma appeared in the early stages. They had blurring of vision and bilateral central scotomas. Their visual acuity after treatment became better (0.8 in affected side and 1.0 in opposite) in four months. The question of surgical treatment remains open under lesions in the top area of the orbit, a possible high risk of injury to the optic nerve.
Final case is a patient G (Figure 3), who had heavy multiple fractures of the lower and outer walls of the orbital displacement, a crack in the region of the orbit apex. His preoperative visual acuity was low (0.04 in the affected side and 0.6 on the opposite side). He also took intravenous infusion of Methylprednisolone in dose 1000 mg one day before, at the same day and two days after the operation. Later dose of steroid was reduced gradually. Currently, three months after injury acuity in both eyes was 1.0. Optic nerve lightness of the right eye and the increase in electrical sensitivity threshold remain insignificant.
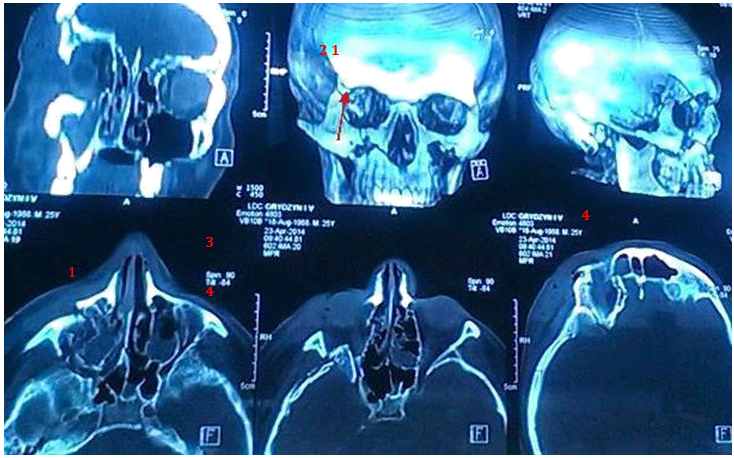
Figure 3 MRI of patient G.: the multiple fracture of lower (1) and lateral (2) walls of right orbit associated with the optic nerve compression of right eye (3) in orbital apex (4). Heavy multiple fractures of the lower and outer walls of the orbital displacement, a crack in the region of the orbit apex. Preoperative visual acuity was low (0.04 in the affected side and 0.6 on the opposite side).
Neuroprotective treatment for the compressive traumatic optic neuropathy will help to protect the optic nerve from possible repeated injuries. This will increase the effectiveness of general treatment if the final conclusions will be adjusted in view of the importance of this approach to treatment requires more extensive research in the future.
None.
The author declares there are no conflicts of interest.

©2016 Moyseenko. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.