Advances in
eISSN: 2377-4290


Case Report Volume 12 Issue 2
1FAAO, National Eye Centre, Pakistan
1FAAO, National Eye Centre, Pakistan
2Ophthalmology, King Edward Medical University, Pakistan
2Ophthalmology, King Edward Medical University, Pakistan
Correspondence: Dr. Rubina Shah, FAAO, King Edward Medical University, Lahore, Pakistan, Tel 03424-014487, Tel 03424-014487
Received: June 08, 2022 | Published: July 18, 2022
Citation: Shah R, Wali K. A cutting-edge refractive surgery treatment option for Forme Frust keratoconus. Adv Ophthalmol Vis Syst. 2022;12(2):36-41. DOI: 10.15406/aovs.2022.12.00414
Forme Fruste keratoconus is a keratoectatic condition of keratoconus that is a rare, unilateral subclinical, abortive, and unusual syndrome. This case outlined a brief discussion of moderate cornea deformation due to mechanical form by prolonged contact lens use dominantly in one eye. It showed topography’s efficacy in discriminating clinical indices to determine corneal mild ecstatic condition, mainly by a practioner. Forme Fruste keratoconus associated with the mild refractive error may benefit from refractive surgery. Meticulous care must be considered before evaluating the preliminary examination of refractive surgery.
Keywords: forme fruste keratoconus, ocular dextrus, ocular sinister, keratoconus, best fit sphere, keratoconus probability index, cone location magnitude index
A 26-year-old Asian female presented for a complete preliminary examination for refractive surgery. The primary complaint was a mild irritable eye with blurred distance vision without spectacles. She denied ocular hyperemia, tearing, discharge, and pain. Her previous ocular history showed a ten-year dependency on a soft contact lens of -2.00D. She denied past ocular, contact lens-induced infections, surgery, or trauma. Family ocular history was normal for refractive errors. The patient’s medical history was normal. Social history was normal. She had no known drug allergies. She was oriented to time, place, and person.
Uncorrected distance visual acuity was 20/60OD and 20/80 OS. Habitual spectacle correction measured via lensometry was -1.75DS sphere OD, - 2.00DS sphere OS, with N5 for near. Manifest spectacle correction revealed was 20/20 OD with -2.25DS and -2.00/-1.00*150 vision was 20/20p OS. Pupils were equal, round, and reactive. Confrontation fields were full of finger counting in both eyes. Extraocular muscles were unrestricted in all gazes without pain or diplopia. The cover test was Orthophoria at a distance and near. Goldman Applanation tonometry measured 12 mmHg OD and 13mmHg O at 10:18 am. Slit-lamp Biomicroscopy revealed normal adnexa, lids, lashes, puncta, and palpebral bulbar conjunctivae in both eyes. The right cornea showed slightly unstable tear film. She denied Vogt’s striae and Fleischer ring of cornea. The Siedal test was normal. Both anterior chambers appeared quiet without evidence of cell or flare; estimation of the chamber angles was 4/4 via the Von Herrick method. Both irides were flat and brown. After dilation, Pupils were dilated using one drop of 1% Mydriacyl showed a normal lens in both eyes. Detail fundus assessment revealed normal optic nerve contour with a cup-to-disc ratio of 0.30 OD and 0.3 OS cup-to-disc ratio neuroretinal rim. The macula showed OU was normal macular reflex with the healthy color of fund.
Diagnosed the disease
One imaging modality was used to study the case. The system running on examination provided Keratometric, keratoconus reports, and corneal biomechanics properties as an essential tool to diagnose the case. Although the patient was asymptomatic in both, they showed a corrected distance visual acuity of 20/20. The patient was advised to preoperatively undergo routine corneal topography with the G4 (Galilei) Ziemer system to assess corneal deformation. Early keratoconus changes with astigmatism of 0.2DC OS and 0.18DC OD with manifest refraction mild myopic refractive error 2D. Corneal Topography showed elevation and curvature of both anterior and posterior corneas on curvature-based topography and topography, which has been the most popular tool to evaluate early changes in contemporary techniques. It also calculated the Pachymetry profile, thus interpreting enormous complexity. It optimized the ability to detect minor ectasia of corneal surface by extrapolating topographic maps, which are misused mainly by simply evaluating from the K-value. The diagrams illustrated focal steepening in post-elevation-based based topography and corneal biomechanics. The below case was interpreted with comparative another case with normal one eye and marked early keratoconic corneal steepening skewing bowtie as shown in Figure 6.
Diagnostic tools to rely on
In 1980 the first video keratography was introduced for keratoconus. Plascido disk images were used in this system to analyze anterior corneal curvature. Similarly, various zones of corneal power, superior-inferior asymmetry, and multiple corneal biomechanics were introduced to assess keratoconus. To discriminate keratoconic eye from several normal indices were developed with progression, thus improving the sensitivity of these tests. Klyce-Maeda group and the Rabinowitz introduce KISA% percent valuate keratoconus probability.1,2
In recent years, elevation-based topography gained more popularity in assessing the deformation of the cornea. The slit scanning technique and scheimpflug technique is used as Orbscan and Pentacam are widely used in the USA. And, Scheimpflug is commonly used in a variety of instruments: The Pentacam (Oculus, Arlington, WA, USA), the Galilei (Ziemer Ophthalmic Systems AG, Port, Switzerland), the Precision (Ligi Tecnologie Medicali, Taranto, Italy), and the Sirius (CSO Ophthalmic, Instrument Company, Auckland, New Zealand).
The apparent map of elevation-based topography over curvature base is that it covers a more detailed area of the cornea than vediokeratogrpagy. Hence, a larger diameter allows peripheral detection of corneal deformation as well. Second, elevation-based topography reduces exaggeration of Kappa angle 5 degrees as increased by normal plascido topography. Further, it measures the posterior curvature of the cornea, where recent studies have shown posterior curvature changes in early keratoconus. As in FFK, the elevation-based topography of the above case could tell deformities tremendously, ignoring normal curvature K- value and visual symptoms.
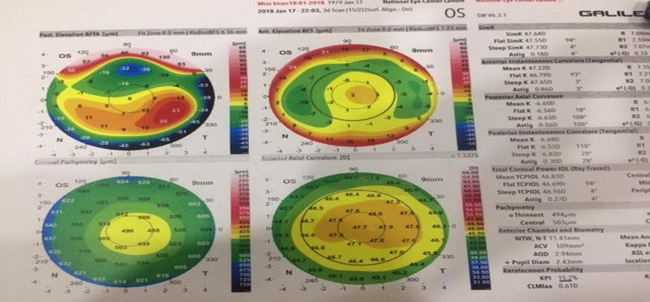
Figure 1 Photo courtesy Rubina shah National eye Centre.
Note: The report clearly showed a localized inferior steepening tongue-shaped but asymmetrical deformation of the posterior elevation map and reduced corneal Pachymetry.
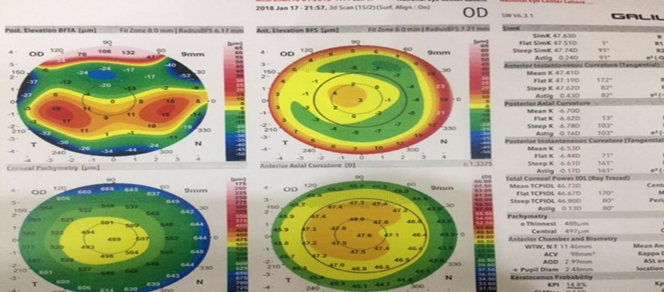
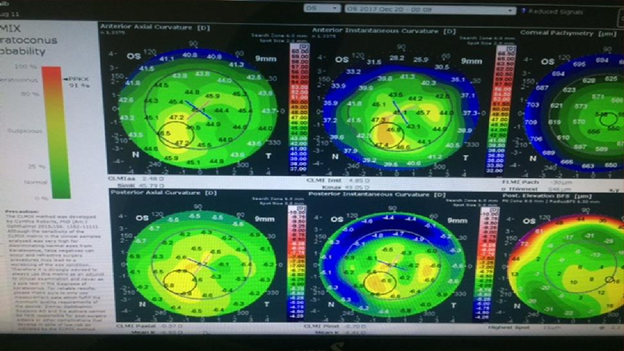
Figure 2 Photo courtesy Rubina Shah National Eye Centre.
Note: BFS (Best Fit Sphere) The posterior elevation of the right eye also showed subclinical changes in keratoconus central island changes in 4-5D steepening and I-S value. Whereas astigmatism is only 0.2D*91 and reduced Pachymetry to 488micron.
Understanding the map
The topographic reports showed Forme Fruste keratoconus FFKC a brief understanding of map interpretation in posterior elevation BFTA and a tongue shape steepening of corneal profile. A good experience with corneal topographic graphs is needed to select a suitable treatment protocol evaluation. Another opinion coincided with the keratoconus suspect with FFKC, which I defined above. Waring3 identified keratoconus suspects as “the fellow eyes of unilateral keratoconus that had no slit-lamp findings.” He distinguished the term keratoconus suspect should extend to “patients with manifest clinical keratoconus in one eye and only video keratographic inferior steepening in the other eye. This case outlined a unilateral eye subclinical KC deformation with an explanation of another patient with the same pattern.
Background of Cornea Optics: An immense optical power of the eye provides by the tear film and air interface. However, normal tear film can have a detrimental effect that can disturb vision markedly—for example, dry eye syndrome and Blepharitis. The anterior corneal curvature determines the eye’s optical power, which produces about two-thirds of the refractive eye power, approximately 48D. The overall power of the cornea is less than 42D as we negate the power of posterior corneal curvature around -6.00D. Standard corneal topography measures the anterior corneal radius of curvature. It extrapolates the cornea's K central power by measuring the curvature change rate from a centrally 4mm zone. That cornea flattens from the center to the periphery makes it very decisive to determine power at a single point. The corneal dimensions are critical to rule out any disease related to the optics and laser procedures to alter the dimensions. Changing the eye's refractive status by 2.00D may vary the corneal thickness by 30 Micron.
Corneal topography estimated the pattern of the axial map, anterior and posterior elevation (float) maps, and corneal pachymetry
Axial map: Axial power represented the supposition that the cornea is a sphere and that angle of incidence of an instrument is normal to the cornea.4 It is based on the axial distance representing the average corneal power, thereby providing a smoother representation of curvature and power of only central 1-2mm. Topographic maps display the curvature and power are a natural sense of physiological flattening of the cornea, but it does not reflect the true power of the peripheral cornea. Hence, this map is not a good description of corneal topography. The Diagram showed the curvature difference in Forme Fruste keratoconus without any marked variations in diopters of K readings of anterior axial curvature as shown in patient reports. It underestimates steeper curvatures and flatters curvatures due to dependence on the reference axis. However, it fails to describe the true shape and power of the peripheral cornea.
Tangential map: The second method of describing corneal curvature is instantaneous radii of curvature. It determines the curvature by a tangent path from a point to the plane that intersects the point and visual axis. The map typically shows a better sensitivity to peripheral changes with less curvature smoothing than the axial map. For screening purposes, most surgeons prefer axial output then tangential mode.
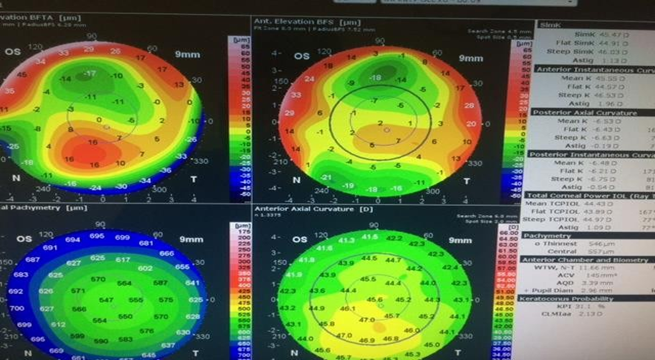
Figure 3 Diagram illustrated anterior axial curvature with normal Keratometric value and astigmatism 1.13DC whereas anterior elevation peripheral steepening.
Elevation maps: Elevation of the cornea is defined as the elevation of the cornea in reference to the” best fit sphere.” Although it doesn’t measure elevation, it gathers elevation data by reconstructing measurements using sophisticated algorithms. It defines the height by measuring microns.5,6 The map showed localized tongue shape deformation elevation of posterior corneal curvature with 16micron OD steepening from normal 12D. The map represents the color of steep areas due to mechanical changes associated with prolonged contact lenses.
Differential diagnosis:
Corneal warpage corneal warping shows a dramatic topographical alteration due to prolong contacts wearer markedly in a rigid gas permeable contact lens. The corneal topographical maps typically show the bilateral and symmetrical superior flattening and dramatic inferior steepening. And characteristic “scissors-reflex” is seen in retinoscopy. It is caused by a rigid fit lens decentered superiorly, and a spherical rigid contact lens is worn on the moderate toric cornea. However, with the recent availability of highly Gas-permeable materials, improved lens designs, and complex corneal mapping systems, corneal integrity and shape can be maintained and monitored to reduce corneal warping and severity.
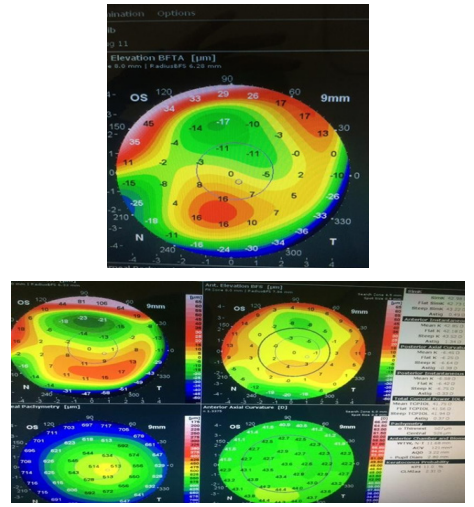
Figure 4 FFKC with marked corneal alteration topographic profile and reduced Pachymetry right eye with mild, regular astigmatism.
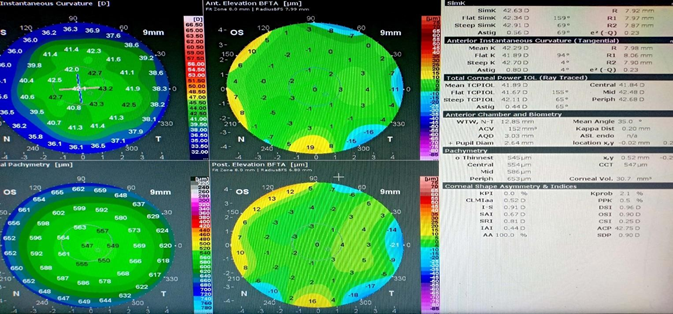
Figure 5 Clinical Topographic report of the same patient with unaffected vision, corneal biomechanics, and normal topography.
Note: CLAMx report showed apparent keratoconic changes with PPK 91% with asymmetric skew irregular steepening inferiorly as topographic alteration. There was a marked change in posterior instantaneous 6D to 4D diopter values. As shown in the figure.
Corneal Pachymetry and biomechanics:
Corneal Pachymetry and biomechanics: Corneal Pachymetry decreased by 507-micron OS and 545 OD. The keratoconus probability index of Keratoconus was 15% or 31% OD and 11% OS, respectively.
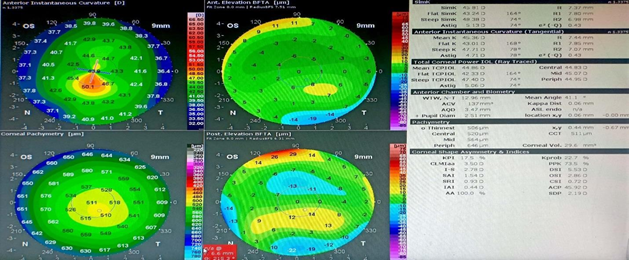
Figure 6 Another patient without any history of contact lens use showed an inferior skewing bow tie elevation map and KPI of 17.5%, Pachymetry 507 (Keratoconus suspect).
Rubbing of eyes:
Constant rubbing of the eye due to allergic and dry eyes can cause deformation of corneal topography.
Post refractive surgery: It is necessary while very evaluating a candidate for laser vision correction, the presence of the mild disease may develop a risk factor for progressive iatrogenic keratectasia. However, the confusion in the literature is that mild (subclinical) disease refers to the same as mild topographic irregularity. In such cases, evidence is incorrect because patients have mild disease with normal front surface curvature and unaffected visual acuity.
Resiliency to trauma: Trauma to the globe can also exaggerate corneal profile.
Finger indentation by technician: Untrained technicians using instruments or finger indentation of the eye and misalignment can also alter corneal biomechanics and topography.
Treatment: The primary treatment protocol for keratoconus is a spectacle, hard contact lenses and corneal cross-linkage, and keratoplasty, which depends on the severity of KC in advance case of KPI >40%. However, patient with FFKC has abnormal topography only without any manifestation and progression of clinical symptoms. A patient with mild refractive error can be treated with corneal refractive surgery. The patient was keen on refractive surgery. A frequent topography visit was planned to see the progression of the disease after another three months. Second, another associated ocular disease such as dry eye tears Systane eye drop was prescribed four times a day to attain normal corneal tear film. The patient was temporarily comfortable with spectacles therapy, and the soft contact lens was stopped to avoid further deformation due to warping.
The patient was guided about the disease as a wrong indication for refractive surgery in higher- aberrations. Consequently, refractive surgery can aggravate visual symptoms in higher-order aberrations. The patient was guided to have sustained regular checkups. Moreover, recent studies show Forme Fruste keratoconus with mild refractive error can be treated with PRK (Photorefractive keratectomy). It is an effective procedure for improving uncorrected vision in patients with mild refractive errors. So, this patient had undergone PRK at National Eye Center in both eyes after follow-ups. Further, close follow-up of patients was guarded to attain confidence regarding further treatment. Six months follow-up was achieved to protect the visual prognosis and assess the overall corneal parameters.7 The patient was satisfied with the visual outcome of comfortable distance vision.
Contact lenses: Various contact lens therapies are available alternatively for myopic management. A Hard contact lens with gas permeable contacts isn’t the same old lens. It allows oxygen to pass through the lens and reach the cornea. With advancing technology, GP lenses are designed at thinner and large diameters with consistent edges Whereas soft lenses are designed to reduce edge discomfort, GP lenses provide a good adaptation. The paramount new lens designed known as “Hybrid lenses” has RGP has entered with surrounding soft lens “Skirt” that offer a wearing comfort available in various parameters to fit irregular shape of a keratoconic eye. However, the patient was reluctant to contact the lens, so spectacle therapy was given as a trial for comfortable vision.
Follow up #1:
First, the follow-up examination was 20/20p with spectacles and the same topographic report. Where Ocular media was normal and fundi were within normal limits. The tear film showed normal.
Follow up #2:
Second, follow-up was after three months, and the patient was evaluated for PRK. She denied any corneal deformation progression, and the topography was stable. A consultant ophthalmologist decided to undergo PRK with patient consent. The pre-Operative examination was 20/20p with -2.00DS OD and -2.00/-0.75*150. The patient was treated with the same refraction. Corneal Pachymetry was 456 microns OD and 494-micron OS with residual stroma bed < 400 microns.
Follow up #3:
A frequent follow-up post-PRK was monitored routinely after one day, one week, two weeks, and one month. A comparative scan showed the following results.
Note: The diagram illustrated pre and post-PRK ablation in a patient with asymptomatic FFKC. The table showed no marked deterioration of corneal profile accepts KPI increased dramatically from 14% to 26% OD and decreased from 15% to 10% OS respectively. K-values, Pachymetry, and astigmatism were stable for six months.
To improve the screening efficacy for a clinician, it is always essential to identify the manifestation of keratoconus. Although, the subclinical pattern of the disease shows an indicative topographic characteristic to reach the threshold of suspicion with modern classification. Subclinical keratoconus presents with minor topographic abnormalities and may skip by doctors clinically without any symptoms.8 this uncertainty creates a grey zone in the science of understanding the disease. Additionally, it has been sometimes defined as cornea with normal clinical findings with keratoconus in one eye where another eye always appears normal.9-11
The inherent challenges to be met by the diagnostic devices are essential. The newly introduced point-source assessed the clinical feasibility color-coded LED array corneal topography system in an FFKC to establish comparison methods of clinical evaluation for refractive surgery primarily with the only available tool, the Ziemer topography system. It shows that Plascido disc topography can detect localized steepening of the cornea, thus indicating the first detectable clinical sign to assess KC clinically. Scheimpflug-based topography considers anterior and posterior corneal surfaces with corneal morphology.12 The Galilei system is a non-invasive diagnostic instrument designed to analyze the anterior eye segment characteristics with the posterior surface by plotting detail maps. Different maps like an axial map, tangential map, instantaneous and refractive. Axial maps measure the curvature of radii relative to their axis. Furthermore, minor corneal irregularities may not be visible due to the common axis. Instantaneous maps only determine local radii of curvature at each point. So, it shows detailed the actual geometry of the cornea by drawing tangent planes to individual points. The refractive map measures the refractive power of the corneal surface at each point by using the snells law. Elevation-based topography shows a detailed posterior apex deviation seen in early keratoconus changes.
“Amsler‟ introduced the plascido-based unusual form fruste keratoconus in 1961. The evolution of advancing technologies paved the path to detecting that disease and vastly modified the technique from plascido imaging to computer video keratography introduced in 1980‟s.13 The indices were developed to discriminate keratoconus from normal eyes. Popular ones included the keratoconus prediction index from the Klyce–Maeda group and the KISA index from the Rabinowitz group.14,15 To detect the subtle anomalies and follow the disease progression in clinically normal eyes of unaffected patients with keratoconus unchanged relatives in the 1990s, the emergence of refractive surgeries and the risk of iatrogenic ectasia or unmasking of keratoconus urged the development of newer diagnostic devices aimed at early detection of subclinical keratoconus. The Orbscan (Bausch and Lomb, Rochester, NY, USA) introduced slit scanning technology to provide wide-field pachymetry and anterior and posterior elevation as a Keratometry map. The Orbscan II combines slit scanning with Plascido-based topography analysis to have detailed studies of corneal parameters.16,17 Compared with maximum posterior elevation, the best fit sphere (BFS), irregularity in the central 3 mm and 5 mm zone, and pachymetry have helped discriminate keratoconus suspects.18
Many studies have revealed methods of screening FFKC preoperatively examination in a patient with refractive surgery, but none is efficient. The topographic data analysis remains superior in the interpretation for screen purposes of the cornea. Various topographic mapping patterns of anterior corneal curvature, asymmetrical bowtie, irregular astigmatism, a skewing radial axis, and abnormal anterior corneal curvature steepening were suggestive that corneal ectasia could be reduced by maintaining a residual stromal bed of 250 microns during corneal refractive surgery.19,20 However, analysis of corneal morphology and biomechanics for the anatomical guidelines during photo ablation is necessary but sufficient. Many publications reported post-refractive keratectasia with more than 250-micron residual stoma with 49% FFKC.21 Biomechanical properties vary pre and post-corneal refractive surgery photoablation procedure. It modifies the intrastromal strength and viscoelastic properties, where the keratectasia condition develops due to alteration of viscoelasticity of corneal collagen fiber.22-24 hence, this highlights the importance of device patency in measuring corneal biomechanical property to improve predictability and biomechanical weakening induced by the photoablation procedure.
Plascido topography can skip early keratoconic changes that can only be detected from a variation of indices generated from percentage thickness and percentage of anterior and posterior curvature over the cornea. However, a single parameter cannot conclude the sole criteria determine the sole criteria to differentiate a normal from a suspect cornea, as some research studies show that overlap is normal to pathological corneas. Diagnostic criteria for KC are currently based on anterior corneal curvature data.25-27 It does not consider other corneal indices from tomography. The performance of those indices with data provided by Plascido topography can help extrapolate artificial intelligence more sensitively and filter the cornea at risk for refractive surgery. FFKC28 shown in the case distinctly diagnosed pre-operative refractive surgery indices and corneal biomechanics helped plan photorefractive ablation further. Recently, a topography-guided surface ablation method has been an encouraging option to rehabilitate vision in patients with contact lens intolerance associated with Forme fruste keratoconus. It is safe, specifically in low myopia, and mild astigmatism, where care must be taken in patient selection and corneal stability must be guarded. Further, corneal total astigmatism data into applied treatment parameters may improve total astigmatism and visual acuity. The indication for Forme fruste keratoconus to undergo PRK must be stable for six months. However, further studies are required to assess the requirement of photorefractive keratectomy in early keratoconus and low mayopes.29,30 the patient must be advised for the corneal cross-linking procedure if there is a reduction of central corneal thickness and changes in corneal regularities. Corneal cross -linkage can also be advised after refractive surgery procedure based on the progressive change of corneal biomechanics and thickness profile.
Comparing topography results can increase the predictability of corneal imaging to provide a good screening for young adults for early keratoconus changes before deciding on refractive surgery. Moreover, essential care must be taken while screening a good candidate with suitable treatment options by understanding the background knowledge of the modern study of cornea imaging technology and map interpretation. Early keratoconic changes with mild refractive error can benefit from the photoablation procedure. Care must be taken while predicting the biomechanics and morphology of the cornea, as a minor alteration may potentiate negative results with aggravated vision after corneal refractive surgery.
None.
None.

©2022 Shah, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.